In this Chapter

The intersection of opioid abuse, particularly injection drug use (IDU), and HIV is well documented; in fact, IDU is the second most frequent route of HIV transmission.2 Injection drug use, either directly or via sexual contact with an IDU partner, accounts for one-third of the estimated AIDS cases since the beginning of the epidemic, and 18 percent of new infections in the United States.3
Opioids are natural, semisynthetic or entirely manmade drugs that bind to receptors in different parts of the body and are generally used as nonmedical painkillers. Heroin, morphine, fentanyl, codeine, oxycodone, buprenorphine, and methadone are opioids.
With an estimated 2.4 million opioid-dependent Americans,4 opioids are among the most frequently abused drugs.5 And nonmedical pain medication abuse has been garnering a lot of press. It's been featured in the Chicago Tribune and The Baltimore Sun, and on MSNBC. It was a front cover story of USA Today and a feature in Time magazine.
According to a 2010 Substance Abuse and Mental Health Services Administration (SAMHSA) national study, dependence/abuse of pain relievers ranked second (after marijuana) among illicit drug use in the past year. Heroin ranked fifth.5
“If I was still under the addiction of [opioids] . . . I would jump up in the morning and I would forget about the HIV medicine and I would go out and get [high].”1
Prescription pain medications, such as hydrocodone (Vicodin), oxycodone (OxyContin, Percocet), and hydromorphone (Dilaudid), are highly addictive.6 According to the SAMHSA study, 5.3 million Americans reported nonmedical use of prescription pain relievers in the last month.7 And the consequences are growing: "Between 2004 and 2008, emergency department visits involving oxycodone, hydrocodone, and methadone increased 152%, 123%, and 73%, respectively, and the number of fatal overdoses due to opioid analgesics now exceeds those due to heroin and cocaine combined.8 In fact, mortality among illicit opioid users has been estimated at 13 times that of the general population.9
This problem is exacerbated among people with HIV (PWH) who may be using such medications for pain management.
- Receipt of prescription opioids to treat pain is not uncommon, particularly as HIV disease is associated with acute and chronic pain syndromes.10
- Pain threshold as well as drug tolerance may change in people who are addicted to opioids.10
- Greater pain severity has been observed in patients who have HIV disease and a mental health disorder.11,12
- HIV-infected patients with drug histories are also more likely to have high higher levels of pain and symptom distress than non-drug-using PWH.13-15
HIV care providers should, therefore, be aware of the increased abuse of prescription opioids.
High prevalence of co-occurring conditions among PWH requires a coordinated system of care. However, the number of opioid-dependent patients significantly outweighs the number of opioid treatment programs nationwide.10 In fact, only approximately 15 percent of substance users are in treatment.16 This is problematic, particularly as substance use is associated with increased risk of HIV transmission,10, 17 and is a barrier to treatment adherence18-23 and therefore, viral control of HIV.22,24-26
On a broader scale, the financial and social costs of untreated opioid dependence in the United States are estimated to be approximately $20 billion per year, including $1.2 billion in health care costs.27
Opioid dependence is treatable--and buprenorphine is one available option. Drug addiction treatment correlates with decreased risk for HIV transmission and improved health outcomes.17,10
Methadone's effectiveness at reducing opioid abuse has been well established, and for many patients this may be the preferred form of opioid treatment.28-33 Methadone, however, may not be right for all HIV-positive patients seeking opioid abuse treatment. Some patients may have tried methadone and been unsuccessful, may have trouble adhering to the strict structure and regulations of methadone programs, and may feel stigmatized by going to a standalone substance abuse clinic. It may be more difficult for some patients to stay in care when HIV services and substance abuse treatment are fragmented (i.e., at separate locations).34
Understanding Addiction
What Do Opioids Do to the Brain, and Why Are They Highly Addictive?
Opioids release an excess of dopamine into the body. Dopamine is a neurotransmitter (brain chemical) involved with learning, motivation, pleasure, and reward. Opioids change the amount and sensitivity of dopamine receptors and can make people feel euphoric; additionally, opioids can suppress pain and reduce anxiety. Eventually, users require an opioid to continuously occupy the opioid receptor in the brain, or they develop withdrawal symptoms.10,35,36
“Nerve receptors are likely to adapt and begin to resist the drug, causing the need for higher doses. The other side of this tolerance is a physical withdrawal reaction that occurs when the drug leaves the body and receptors must readapt to its absence.” 6
The American Society of Addiction Medicine defines addiction as a disease of brain reward, motivation, memory, and related circuitry.37 Images of the human brain have shown that drug use can change the brain's actual structure, function, and metabolism, sometimes long after drug use has ceased.
Dependence is the physiological change that occurs with drug use, resulting in the need to continue use - or increase dosage - to avoid withdrawal.16 Addiction, including opioid dependence, is considered a chronic, relapsing, brain-related disorder.10,27,38
What Increased Risk Behaviors Are Tied to Opioid Abuse?
HIV-positive patients with substance use disorders have benefitted less from treatment than their non-substance using peers.4 This is, in part, because opioid dependent patients are less likely to be prescribed HIV antiretroviral (ARV) medications and, when they receive ARVs, are more likely to be involved in early discontinuation.4,39 In addition, substance use is associated with increased sexual risk behaviors, increased HIV risk, and poorer health outcomes, and contributes to destabilizing conditions, such as homelessness and mental illness.40 As shown in Figures 1 and 2, approximately 18 percent of new HIV infections are attributed to IDU.3
Figure 1: Estimated Cumulative AIDS Cases by Transmission Route, United States
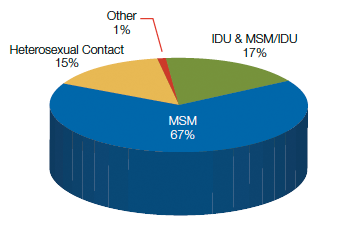
Source: U.S. Centers for Disease Control and Prevention (CDC). HIV Surveillance Report. 2010(22). Table 2b. (Note, percentages may not add to 100 due to rounding).
Figure 2: Estimated AIDS Cases by Transmission Route, United States, 2010
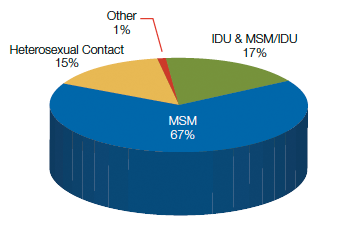
Source: U.S. Centers for Disease Control and Prevention (CDC). HIV Surveillance Report. 2010(22). Table 2b. (Note, percentages may not add to 100 due to rounding).
What Is Medication-Assisted Treatment for Opioid Use?
Medication-Assisted Treatment (MAT) is defined as "the use of medication such as methadone or buprenorphine in combination with counseling and behavioral therapies to provide a whole-patient approach to the treatment of opioid dependence."41 According to an article in JAIDS by Dr. Cheever et al., MAT is an integral component of addressing heroin and prescription opioid abuse alongside HIV treatment and prevention services.10
Why Consider Medication-Assisted Treatment?
HIV primary care clinics facilitate access to opioid treatment in many ways. It can take the form of case finding outreach, referrals from partners and treatment programs in the community, availability of group support and counseling, and access to ancillary services. HIV primary care clinics and community health clinics are already treating many of the health care needs of their opioid-dependent patients. The prevalent model for managing patients with HIV and opioid dependence has been to treat their HIV and substance abuse independently of one another.42 Now, the integration of MAT under the umbrella of comprehensive HIV care services is not only feasible but offers one more way to assist patient needs and create a truly medical home.43
Treatment of opioid dependence results in significant public health benefits — and improved lives and livelihoods for people living with HIV. It allows providers to truly treat the whole person, a hallmark of the Ryan White HIV/AIDS Program. Inclusion of opioid treatment within an HIV primary care setting may also facilitate relapse prevention.44
"A public health policy promoting integrated treatment for HIV [positive] individuals with opioid dependence is [considered] an essential strategy to curb the epidemic."45 This sentiment was included as part of the U.S. Centers for Disease Control and Prevention's (CDC's) Strategic Plan46 and the Health Resources and Services Administration (HRSA) HIV/AIDS Bureau's (HAB's) approach during a groundbreaking Special Projects of National Significance (SPNS) initiative.47 (See SPNS Initiative: Findings from the Field.)