Session Length: 30 minutes
Session Length: 30 minutes
Materials Needed
- Computer and compatible LCD projector to play the PowerPoint presentation
- Paper and easel(s) for taking notes
- Colorful markers
- Tape for affixing paper to the wall as necessary
- Hardcopies of the Module 1 PowerPoint slides (if desired, to be used as a handout to distribute and have participants follow along).
POWERPOINT PRESENTATION
SLIDE 1: Importance of Oral Health Care in Treatment of PLWHA
“You don’t want a healthy neck-down body. You want a healthy top of the head to the tip of the toe body.” — Dr. Howell Strauss, Executive Director of AIDS Care Group of Chester, Pennsylvania, a SPNS Oral Health Initiative grantee
Source Credit: This module on “The Importance of Oral Health in Total Patient Care” was adapted, in part, from a presentation prepared by Stephen N. Abel, DDS, MS, for the AETC National Resource Center.
SLIDE 2: Oral Health and Systemic Health
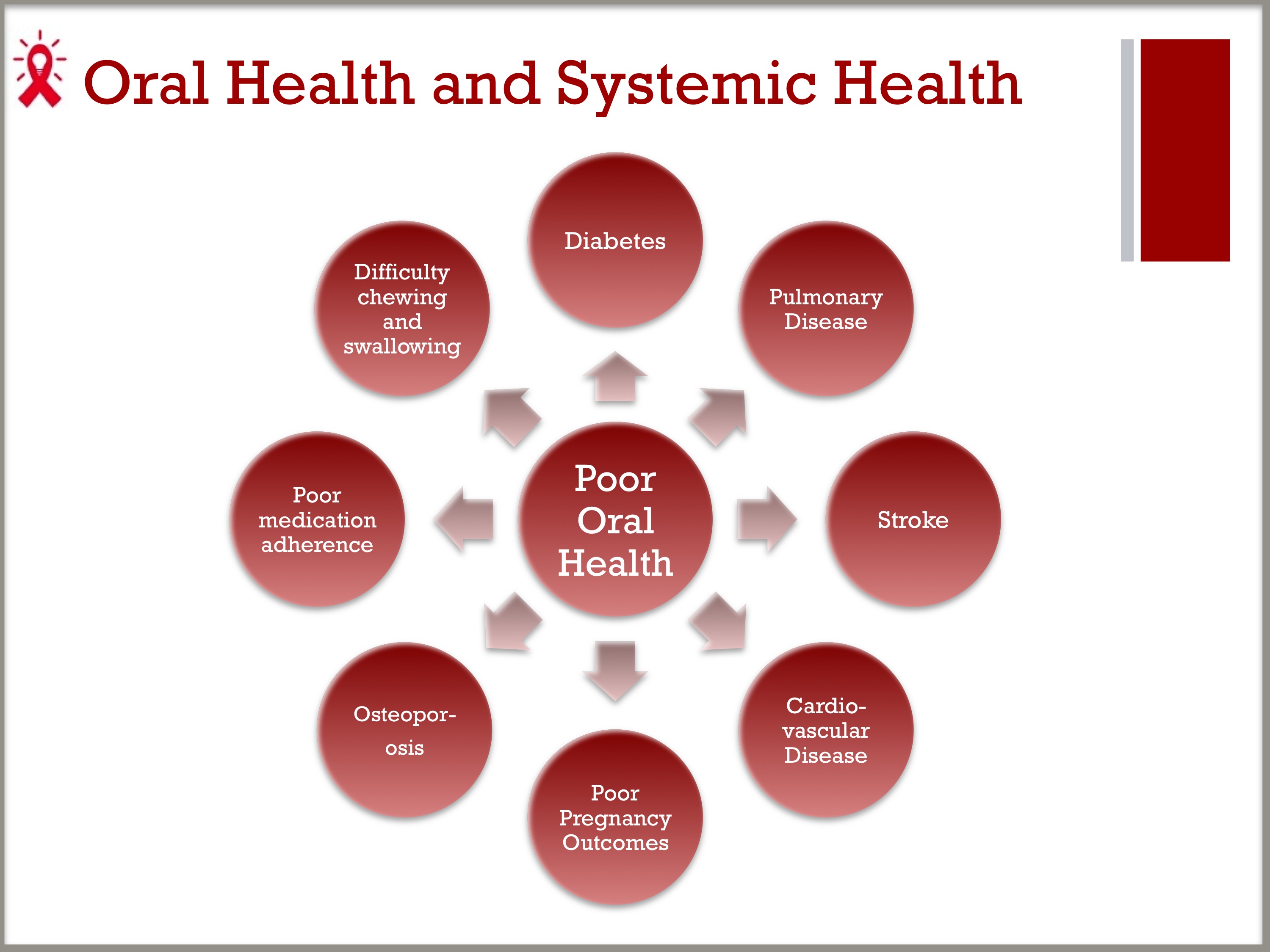
- Emerging research indicates some links between oral health and systemic diseases.
- Recent reports have shown associations between poor oral health—mainly periodontal disease and tooth loss—and increased risk of cardiovascular disease, stroke, pulmonary disease, diabetes, poor pregnancy outcomes, and osteoporosis.
- Poor oral health can make it difficult to chew or swallow and can impede food intake, appetite, and nutrition, leading to poor absorption of HIV medications and leaving PLWHA susceptible to progression of their disease. Poor oral health can also interfere with medication adherence.
- Oral signs suspected to be indications of systemic illness might be confirmed by the presence of rash, fever, headache, malaise, enlarged lymph nodes, or lesions.
- Because there can be a large overlap in the clinical appearance of oral/facial manifestations of various diseases with different etiologies, an accurate diagnosis may require other diagnostic testing.
- More will be explored in Module 5, “Clinical Guide to Integrating Oral Health Care in the Medical Setting.”
SLIDE 3: The Impact of Xerostomia or “Dry Mouth”
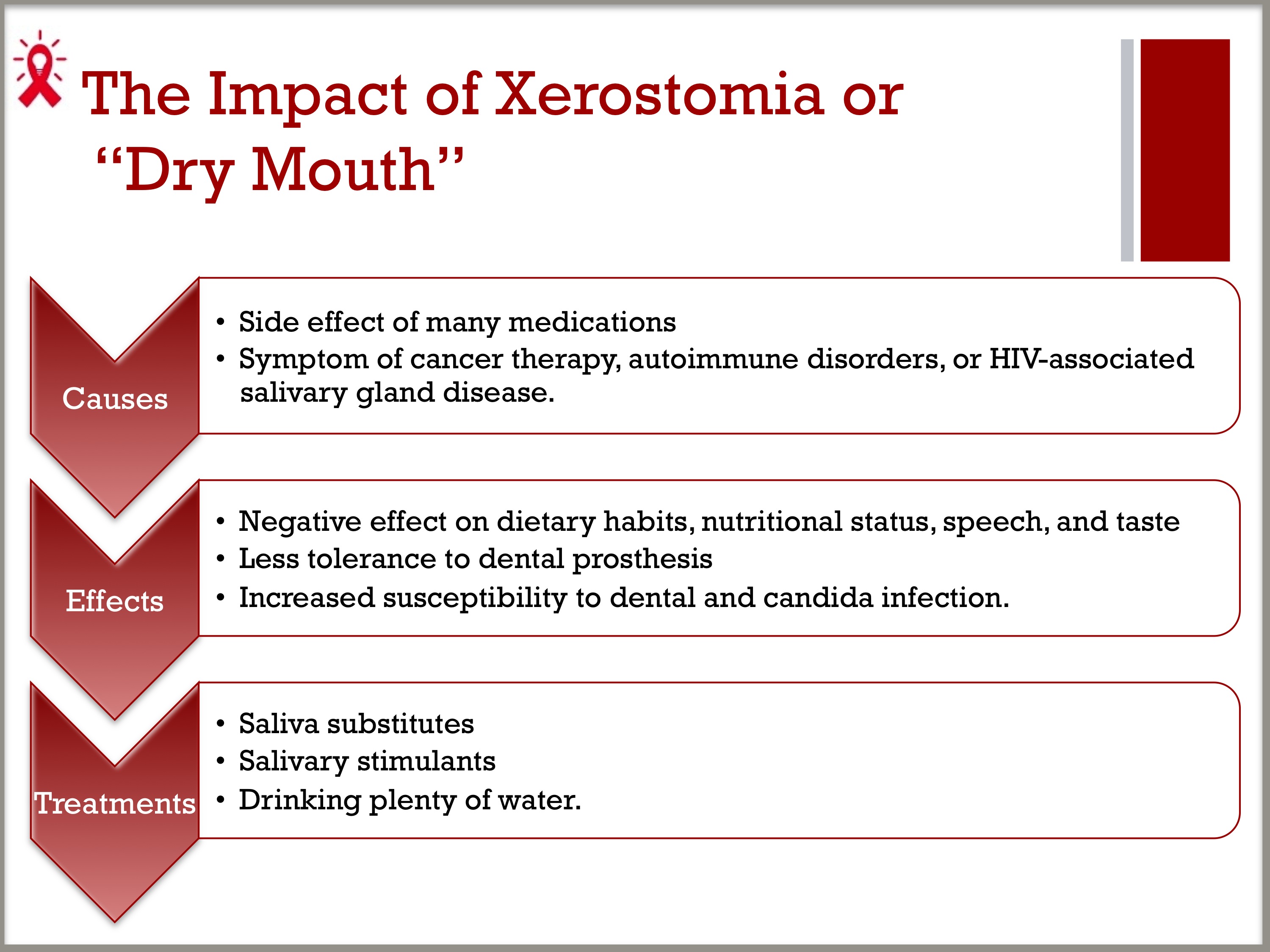
- Xerostomia, also known as “dry mouth,” is not a disease itself, but can be a symptom of certain diseases and a side effect of many medications.
- Xerostomia can produce serious negative effects on patients’ quality of life—affecting dietary habits, nutritional status, speech, taste, and tolerance to dental prostheses—and increases susceptibility to dental and candida infection.
- Common causes for xerostomia include many medications, cancer therapy, autoimmune disorders, or HIV-associated salivary gland disease.
- Saliva substitutes, salivary stimulants, and drinking water regularly have all been found to be effective in the management of xerostomia.
SLIDE 4: More than the Mouth: Oral Health’s Impact on Quality of Life
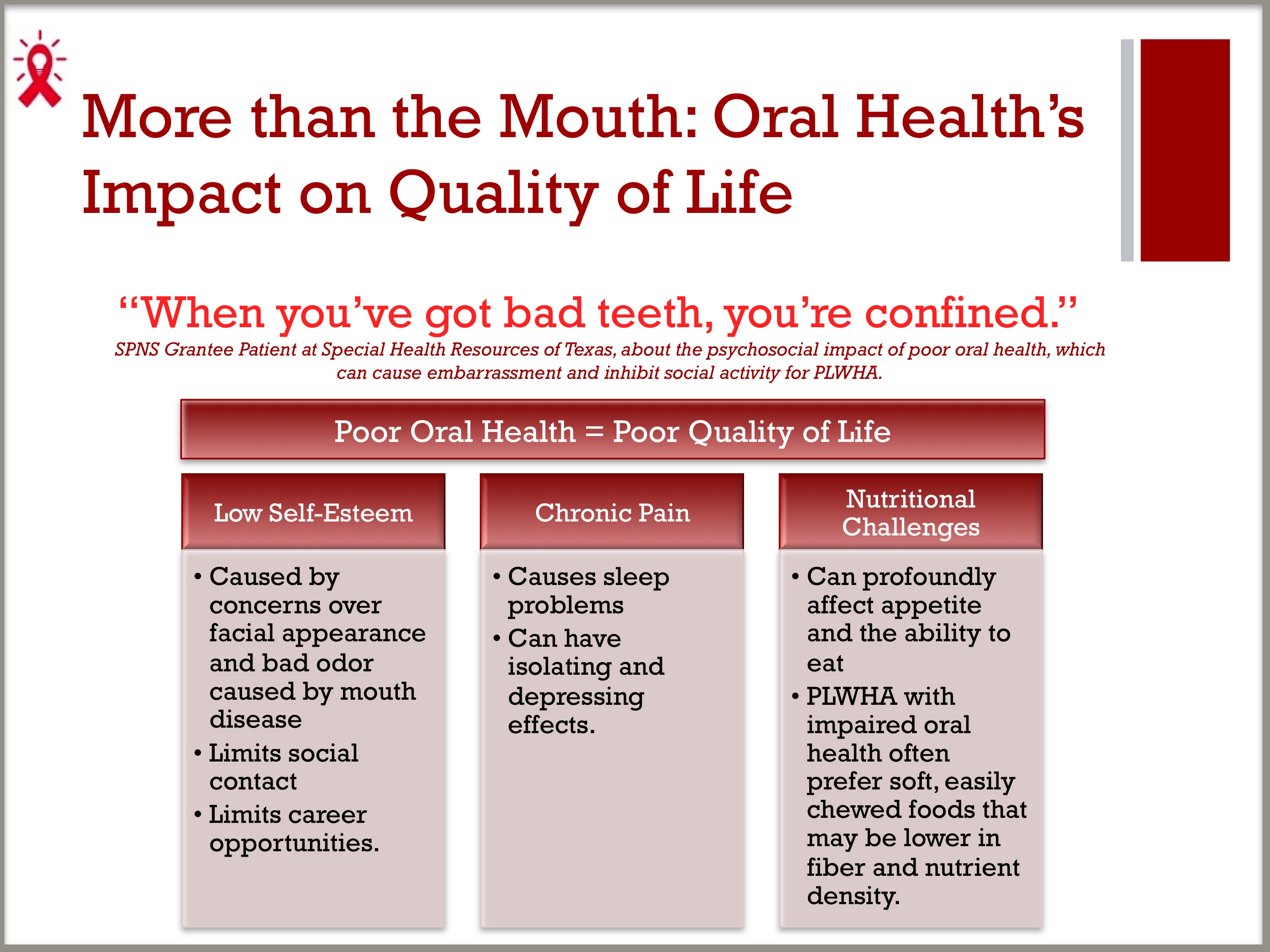
“When you’ve got bad teeth, you’re confined.”— SPNS Grantee Patient at Special Health Resources of Texas, about the psychosocial impact of poor oral health, which can cause embarrassment and inhibit social activity for PLWHA.
- Poor oral health in PLWHA can adversely affect quality of life, lower self-esteem, and limit career opportunities and social contact as result of facial appearance and odor.
- Oral dysfunction can seriously affect nutritional status because it can profoundly affect appetite and the ability to eat. For example, people with impaired oral health often prefer soft, easily chewed foods that may be lower in fiber and nutrient density.
- Sleep problems associated with oral conditions appear to be most closely related to chronic pain, either directly or indirectly in cases where pain and insomnia are exacerbated by depression.
- Oral health problems can lead to avoiding social contact as a result of concerns over facial appearance and bad odor caused by mouth disease.
- Persistent pain has similar isolating and depressing effects.
SLIDE 5: Oral Health and Drug-Regimen Compliance
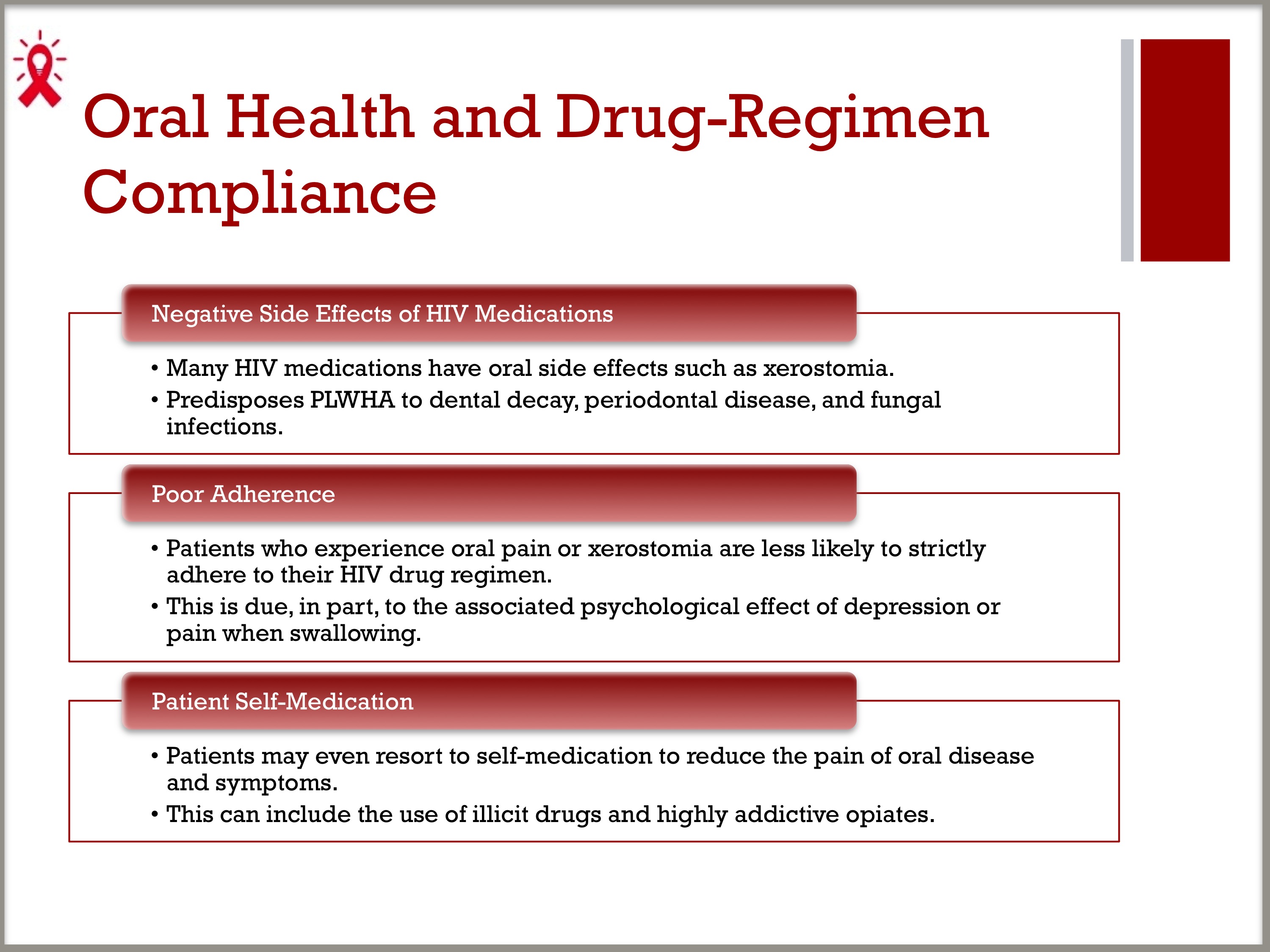
- Many HIV medications have oral side effects such as xerostomia, which predisposes PLWHA to dental decay, periodontal disease, and fungal infections.
- Anecdotal reports suggest that patients who experience oral pain or xerostomia are less likely to strictly adhere to their HIV drug regimen, in part due to the associated psychological effect of depression or pain when swallowing.
- In some cases, patients may even resort to self-medication to reduce the pain of oral disease and symptoms, including the use of illicit drugs and highly addictive opiates.
GROUP DISCUSSION
- Have you seen any of these problems in the PLWHA served by our clinic?
- Which of these problems are most prevalent among the populations we serve?
SLIDE 6: Oral Health Care as a Gateway to HIV Diagnosis and Treatment
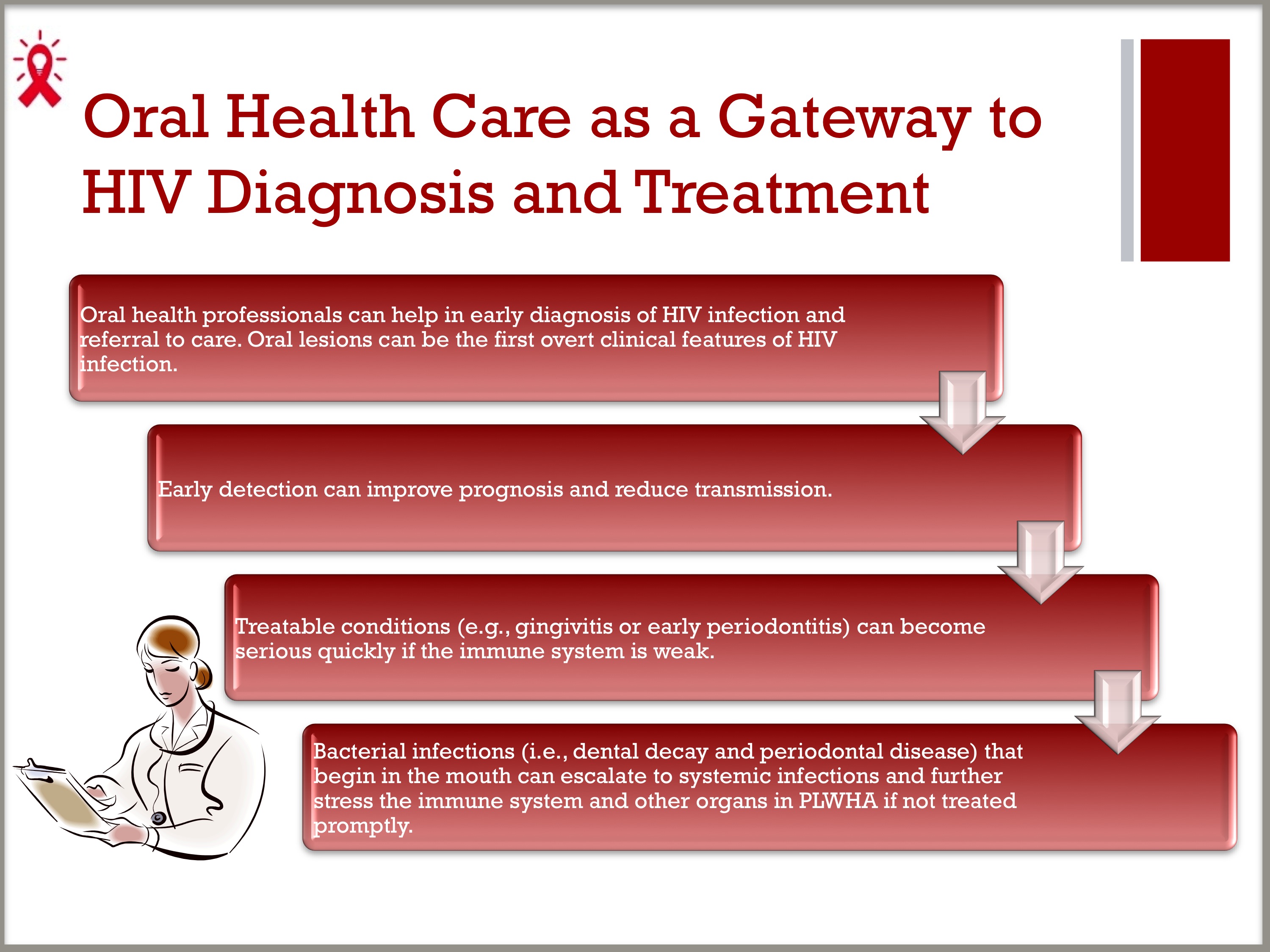
- Oral health professionals can help in early diagnosis of HIV infection and referral to care, as oral lesions can be the first overt clinical features of HIV infection.
- Early detection can improve prognosis and reduce transmission, because infected PLWHA may not know their HIV status.
- PLWHA may find that treatable conditions, such as gingivitis or early periodontitis, can become serious quickly if the immune system is weak. Bacterial infections (i.e., dental decay and periodontal disease) that begin in the mouth can escalate to systemic infections and further stress the immune system and other organs in PLWHA if not treated promptly.
SLIDE 7: Minimum Recommendations for Oral Health Care
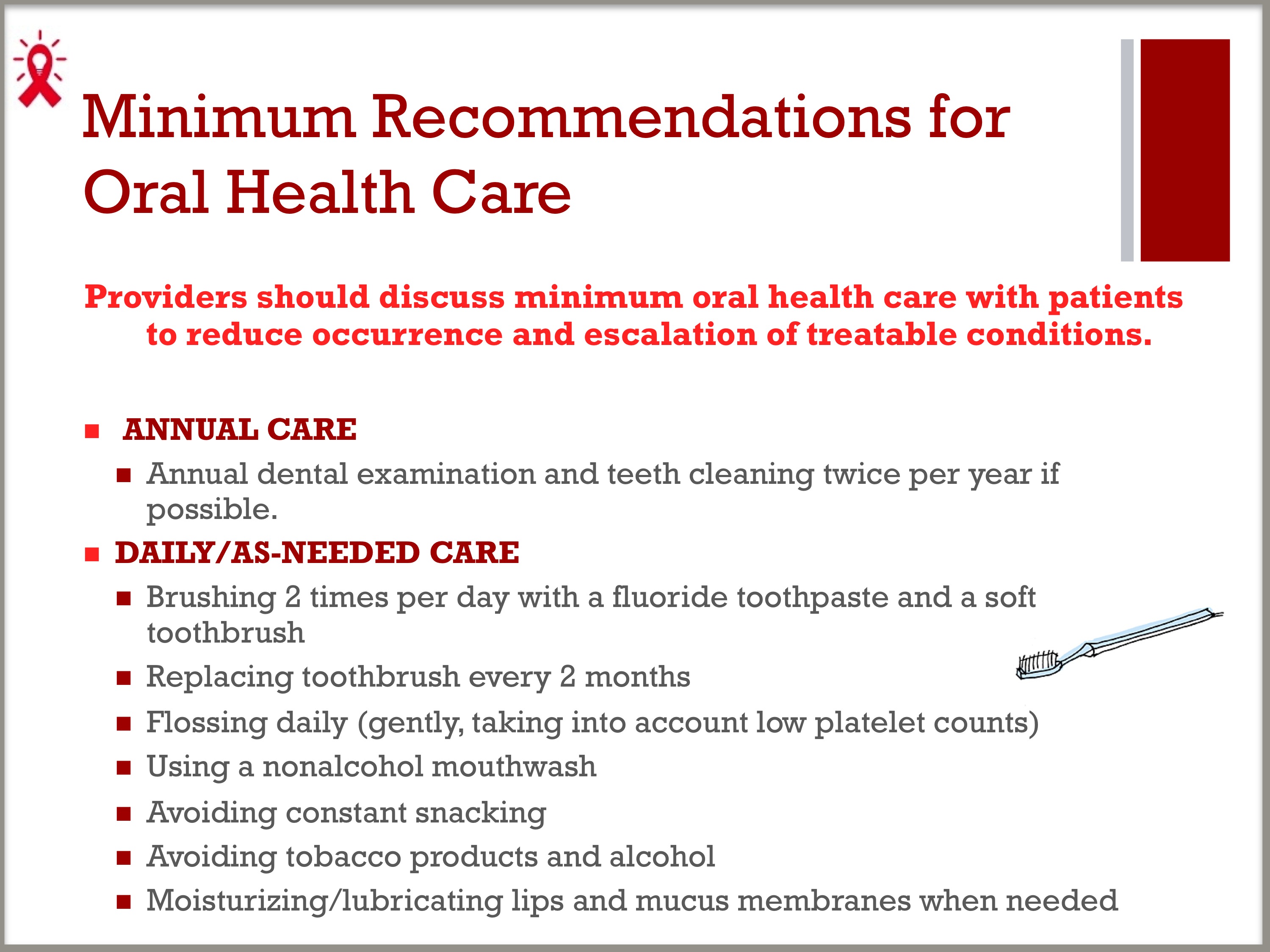
- Providers should discuss minimum oral health care with patients to reduce occurrence and escalation of treatable conditions.
ANNUAL CARE
– Annual dental examination and teeth cleaning twice per year if possible.
DAILY/AS-NEEDED CARE
– Brushing 2 times per day with a fluoride toothpaste and a soft toothbrush
° Replacing toothbrush every 2 months
– Flossing daily (gently, taking into account low platelet counts)
– Using a non-alcoholic mouthwash
– Avoiding constant snacking
– Avoiding tobacco products and alcohol
– Moisturizing / lubricating lips and mucus membranes when needed.
DISCUSSION ACTIVITY
- Have you seen patients referred to HIV care by dental providers, or had patients whose oral health disease was the first outward manifestation of their HIV disease?
- Have you ever had patients ask for oral health advice? Have you ever offered oral health care guidance to patients? If yes to either question, how did you instruct the patient?
- About what oral health care topic do patients seem to know the least? The most?