Session Length: Part 1: 60 minutes; Part 2—Optional Webinar (for in-class training or participant homework): 90 minutes
Session Length: Part 1: 60 minutes; Part 2—Optional Webinar (for in-class training or participant homework): 90 minutes
Summary
This module is designed to provide both visual and descriptive examples of common oral health diseases. At the end of this module, medical providers and primary care staff should demonstrate improved ability to find and identify these diseases in PLWHA.
Materials Needed
- Computer and compatible LCD projector to play the PowerPoint presentation
- Internet connection
- Video player, such as QuickTime (will be required to be installed in advance on your computer)
- Copies of the handout referenced in this module (should be printed out and distributed to each person).
PART 1 (60 minutes)
POWERPOINT PRESENTATION
SLIDE 1: Objective of this Clinical Guide to Integrating Oral Care in the Medical Setting
- Empower medical providers and primary care staff to be able to find and identify common oral health diseases in PLWHA.
Source: Adapted from a presentation prepared by Cesar Augusto Migliorati, DDS, MS, PhD, Professor and Director of Oral Medicine in the Department of Biologic and Diagnostic Sciences at the University of Tennessee College of Dentistry. The presentation is entitled “HIV Diagnosis and the Oral Cavity” and was prepared for the AETC National Resource Center.
SLIDE 2: Diseases of the Mouth as Indicator for HIV Infection
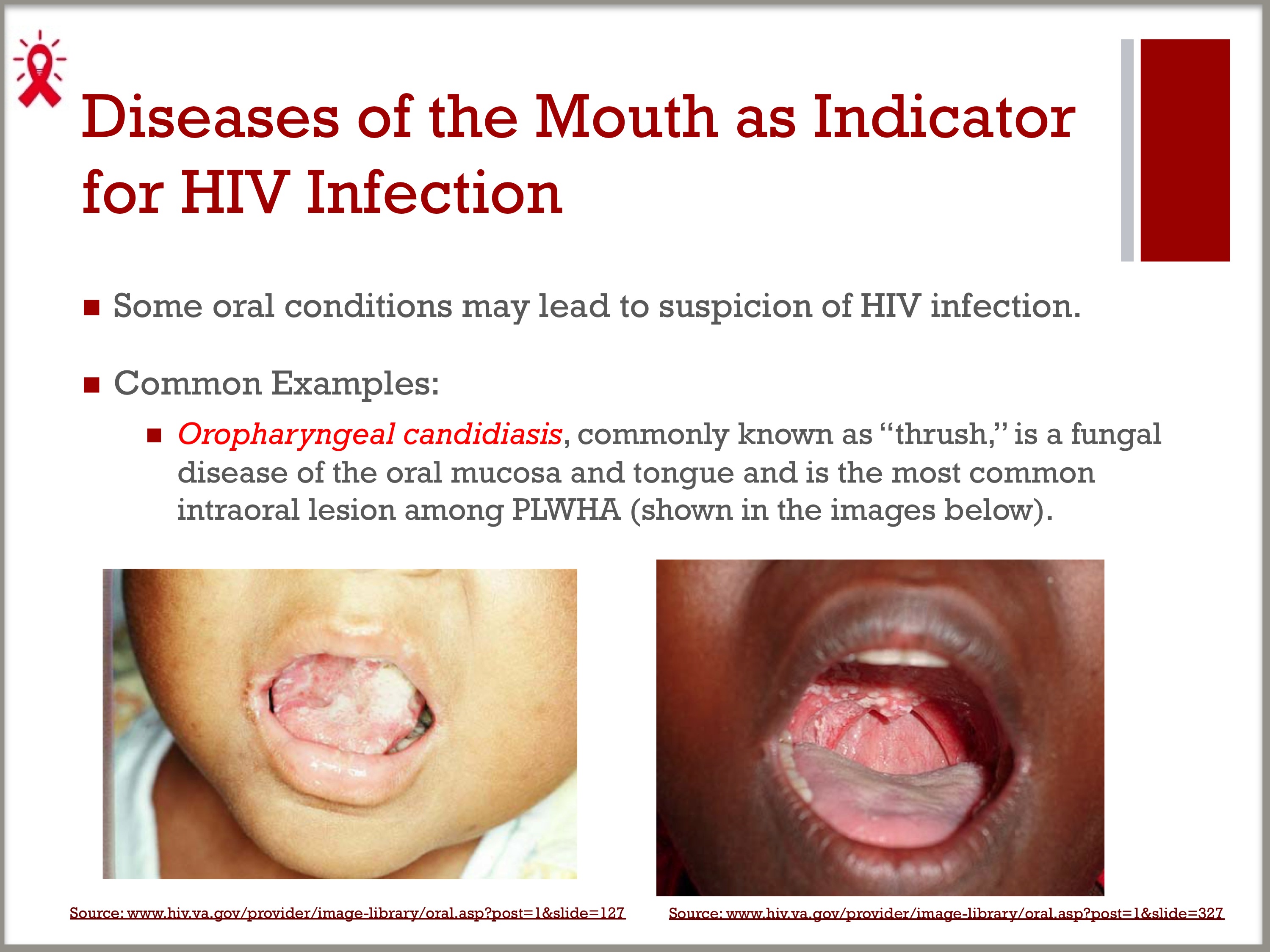
- Some oral conditions may lead to suspicion of HIV infection
- Common examples:
– Oropharyngeal candidiasis, commonly known as “thrush,” is a fungal disease of the oral mucosa and tongue and is the most common intraoral lesion among PLWHA.
SLIDES 2–3: Esophageal Candidiasis
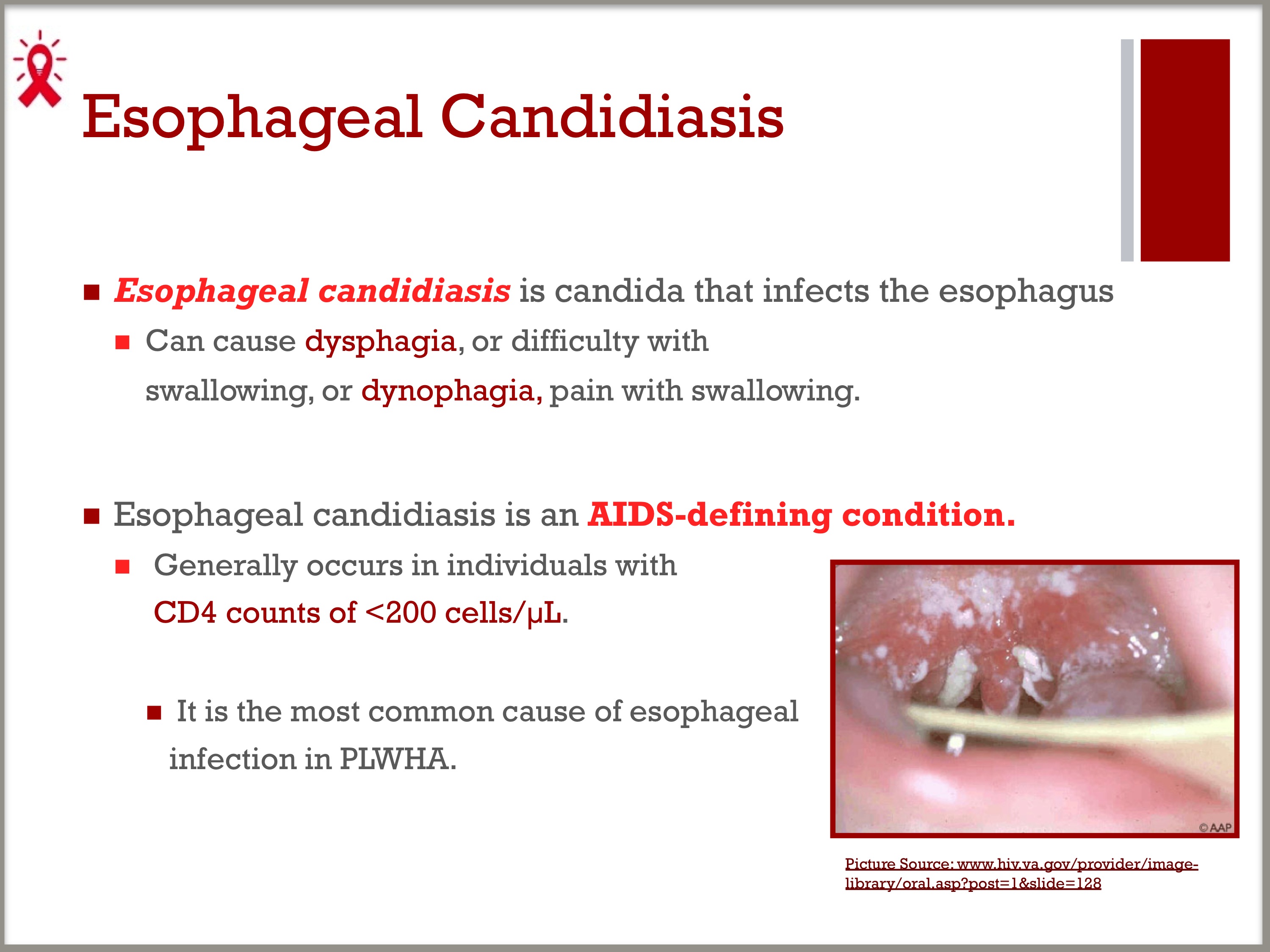
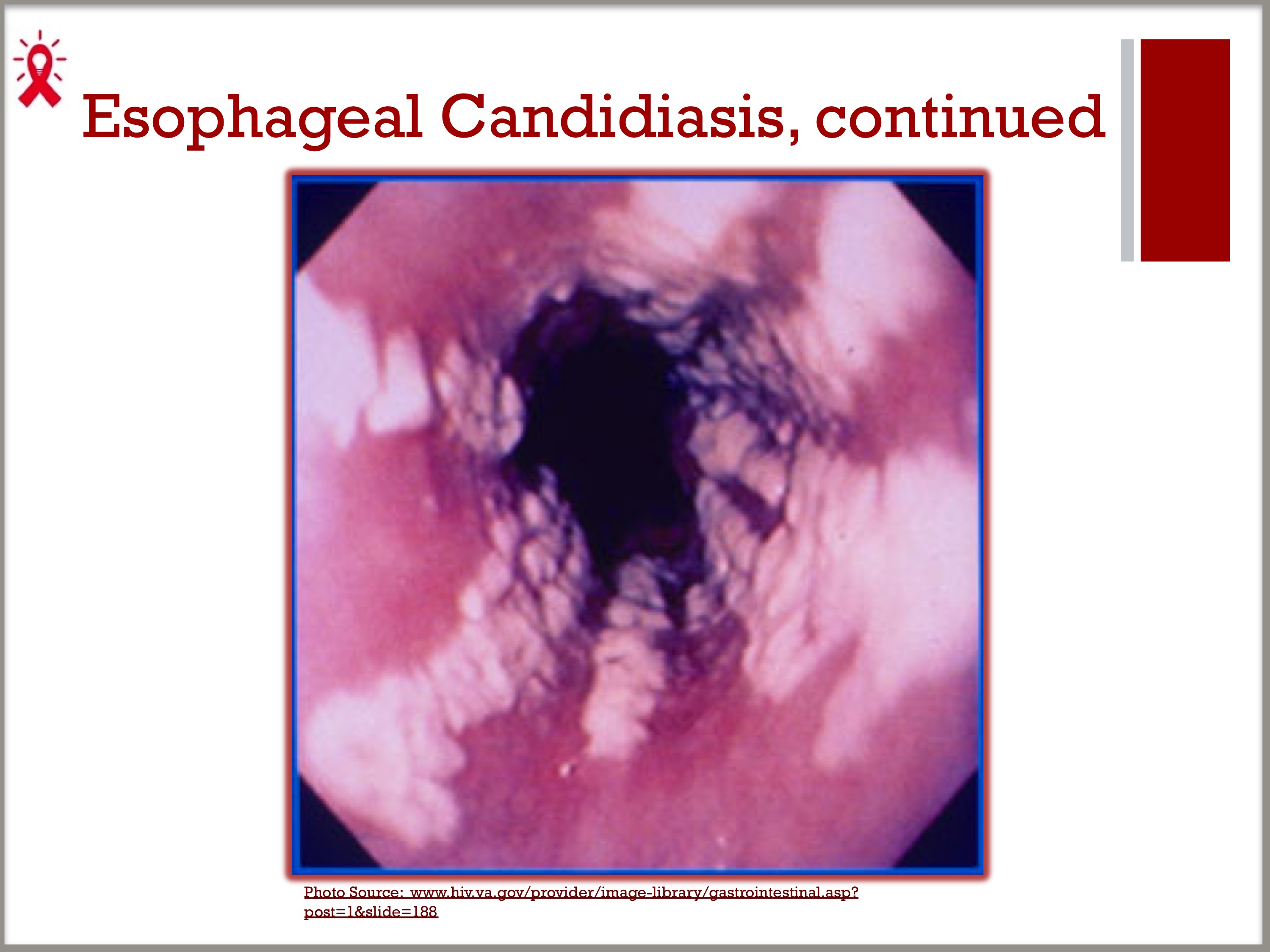
- Esophageal candidiasis is candida that infects the esophagus, which can cause dysphagia, or difficulty with swallowing, or odynophagia, pain with swallowing.
– Esophageal candidiasis is an AIDS-defining condition, generally occurring in individuals with CD4 counts of <200 cells/µL.
– It is the most common cause of esophageal infection in persons with AIDS.
SLIDE 4: Hairy Leukoplakia
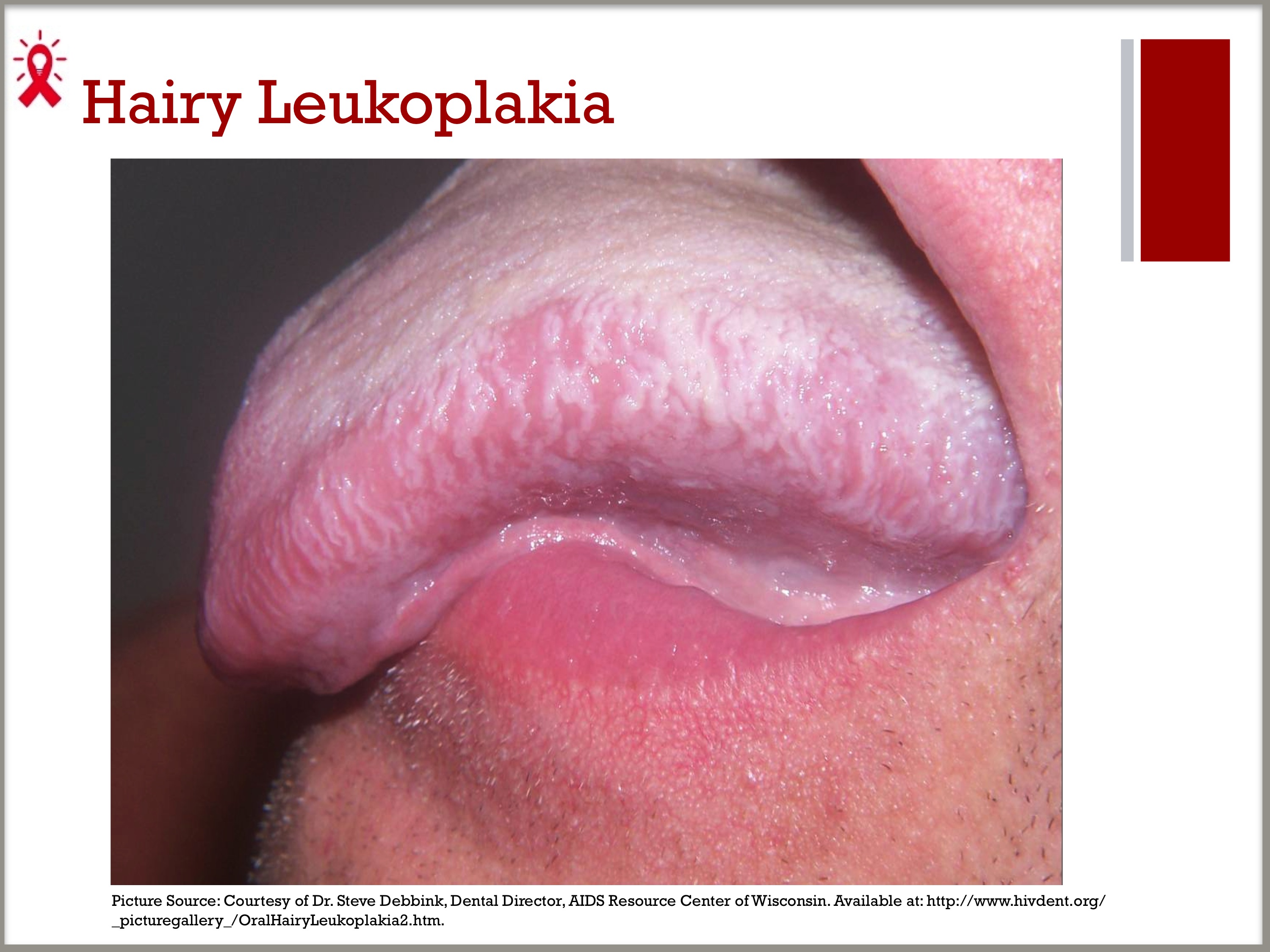
- Before the era of ART, hairy leukoplakia was considered one of the most common oral diseases in PLWHA, occurring in approximately 15 to 20 percent of PLWHA, and is often seen in PLWHA with delayed entry to care.1
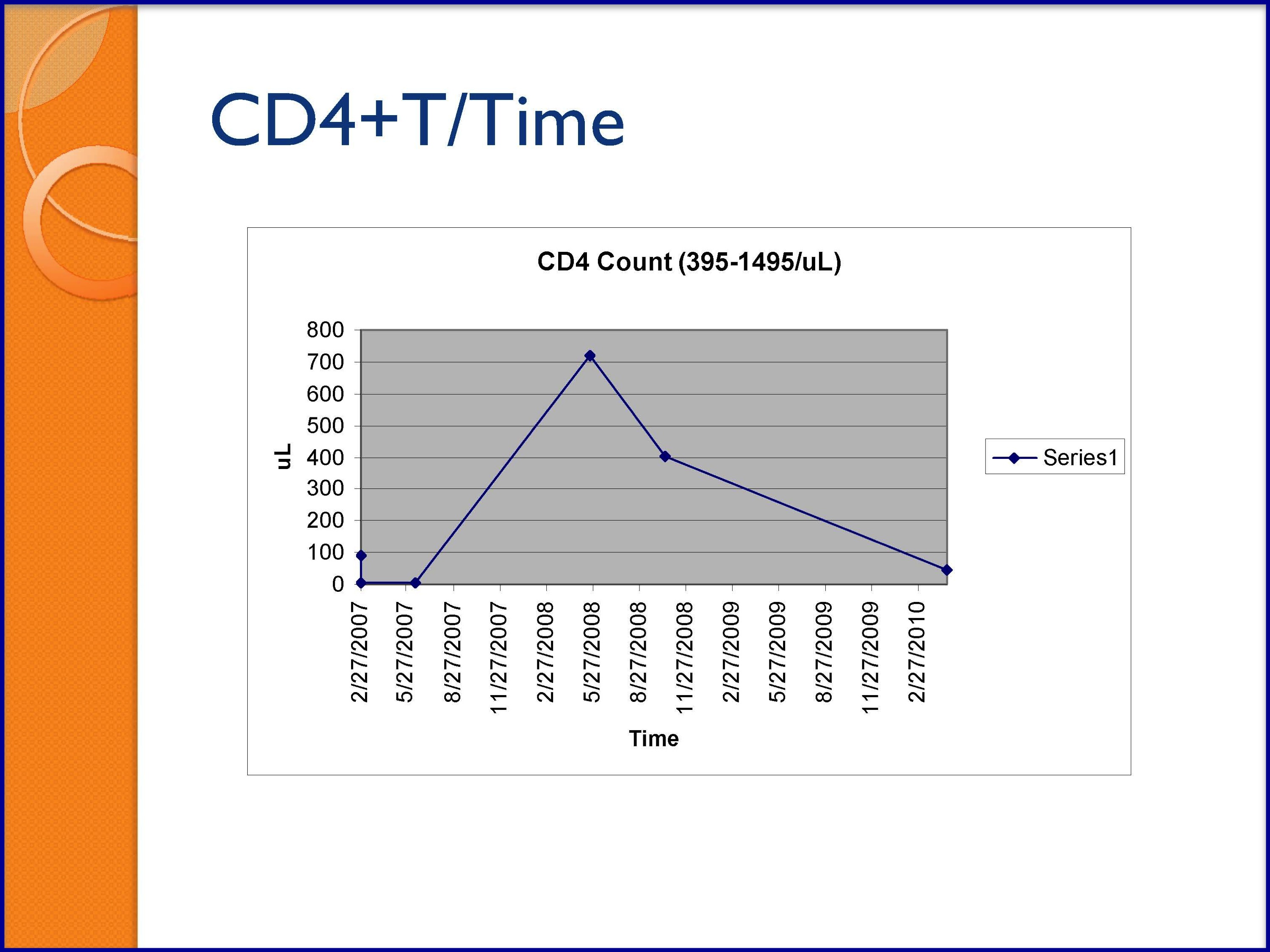
- PLWHA with hairy leukoplakia tend to have moderate to advanced immune suppression, with a median CD4 count of approximately 235 cells/mm3.
1. Husak R, Garbe C, Orfanos CE. Oral hairy leukoplakia in 71 HIV-seropositive patients: clinical symptoms, relation to immunologic status, and prognostic significance. J Am Acad Dermatol. 1996;35:928–34.
SLIDE 5: Hairy Leukoplakia (continued)
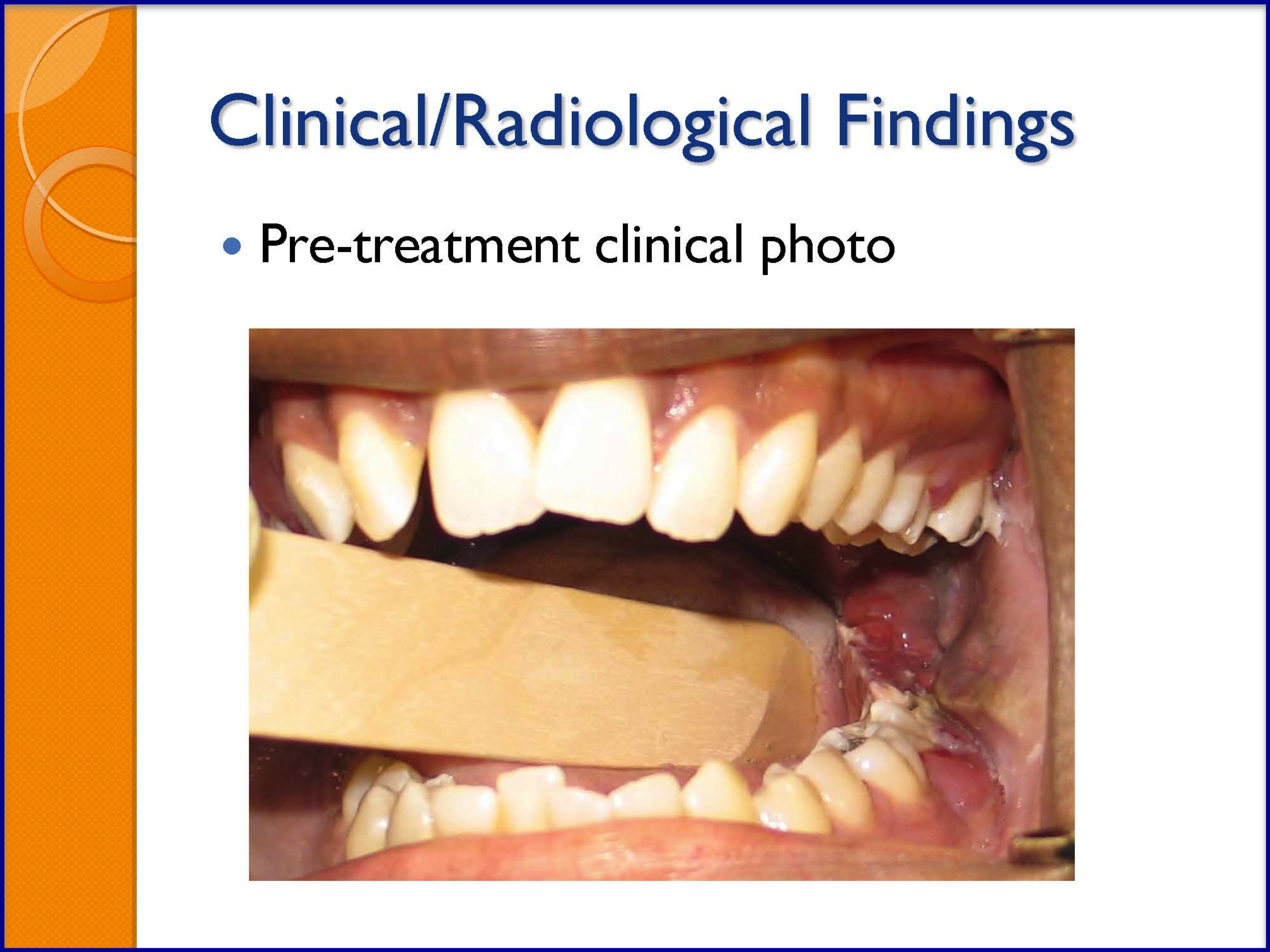
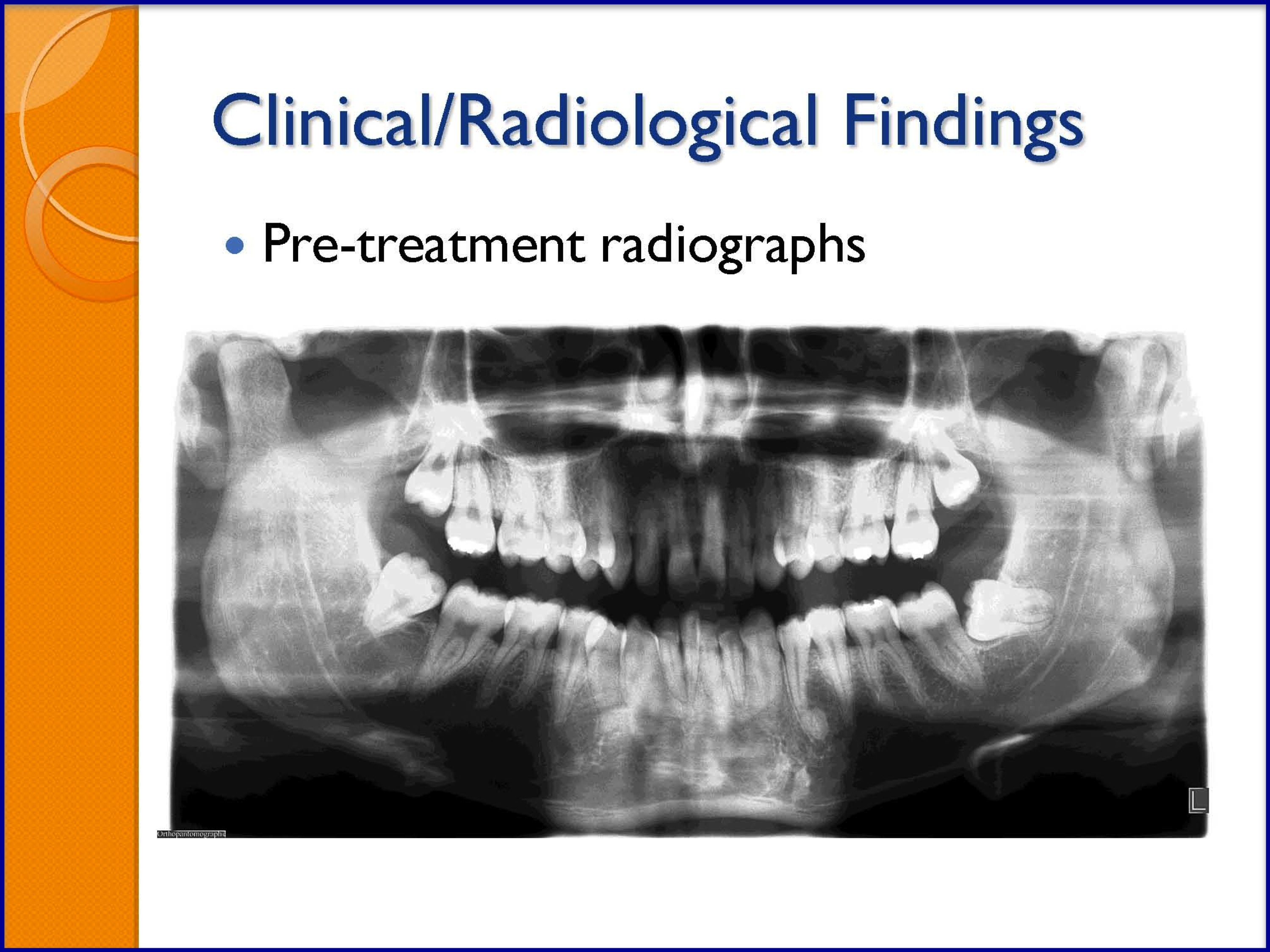
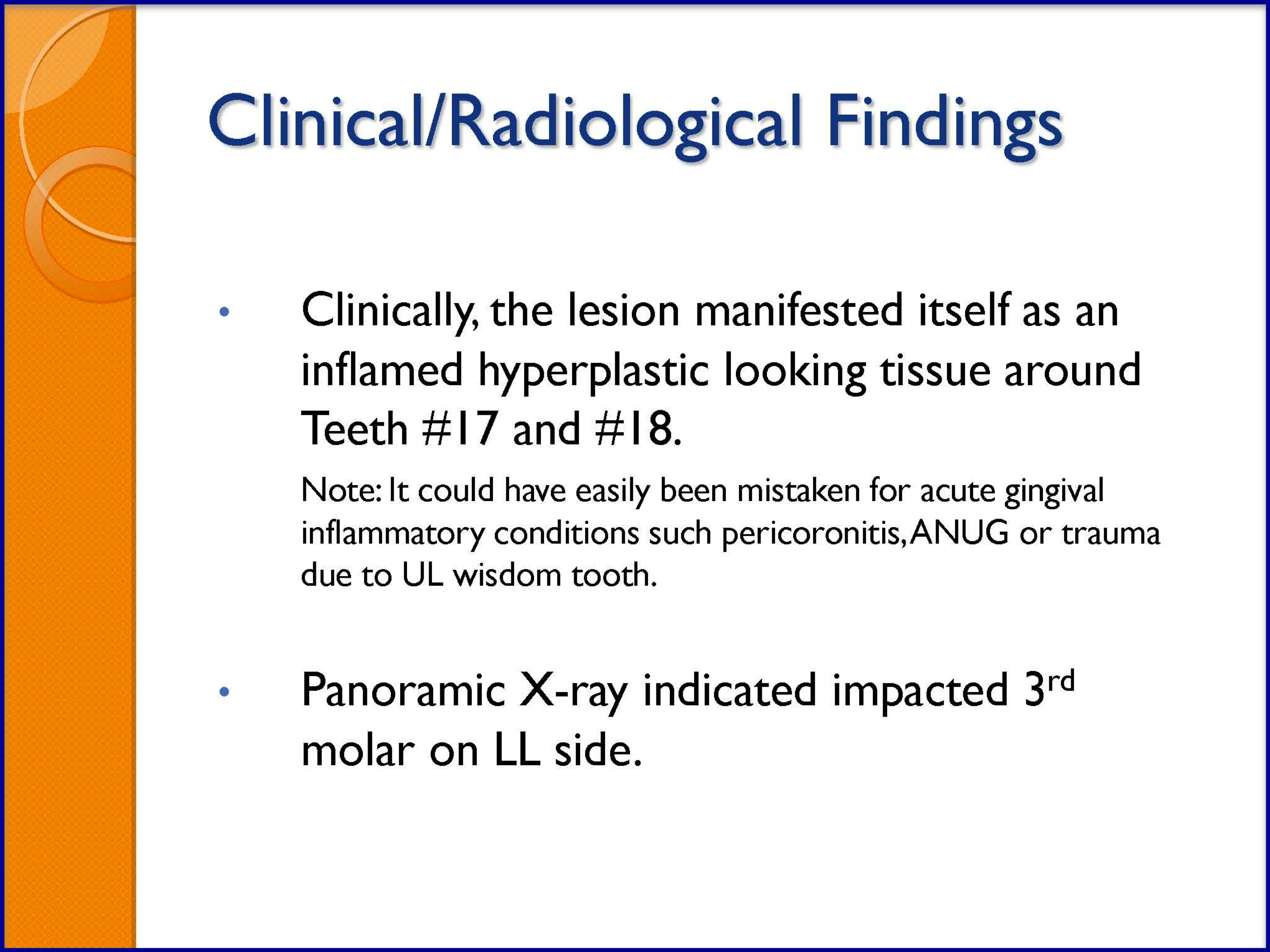
SLIDES 6–7: Kaposi Sarcoma
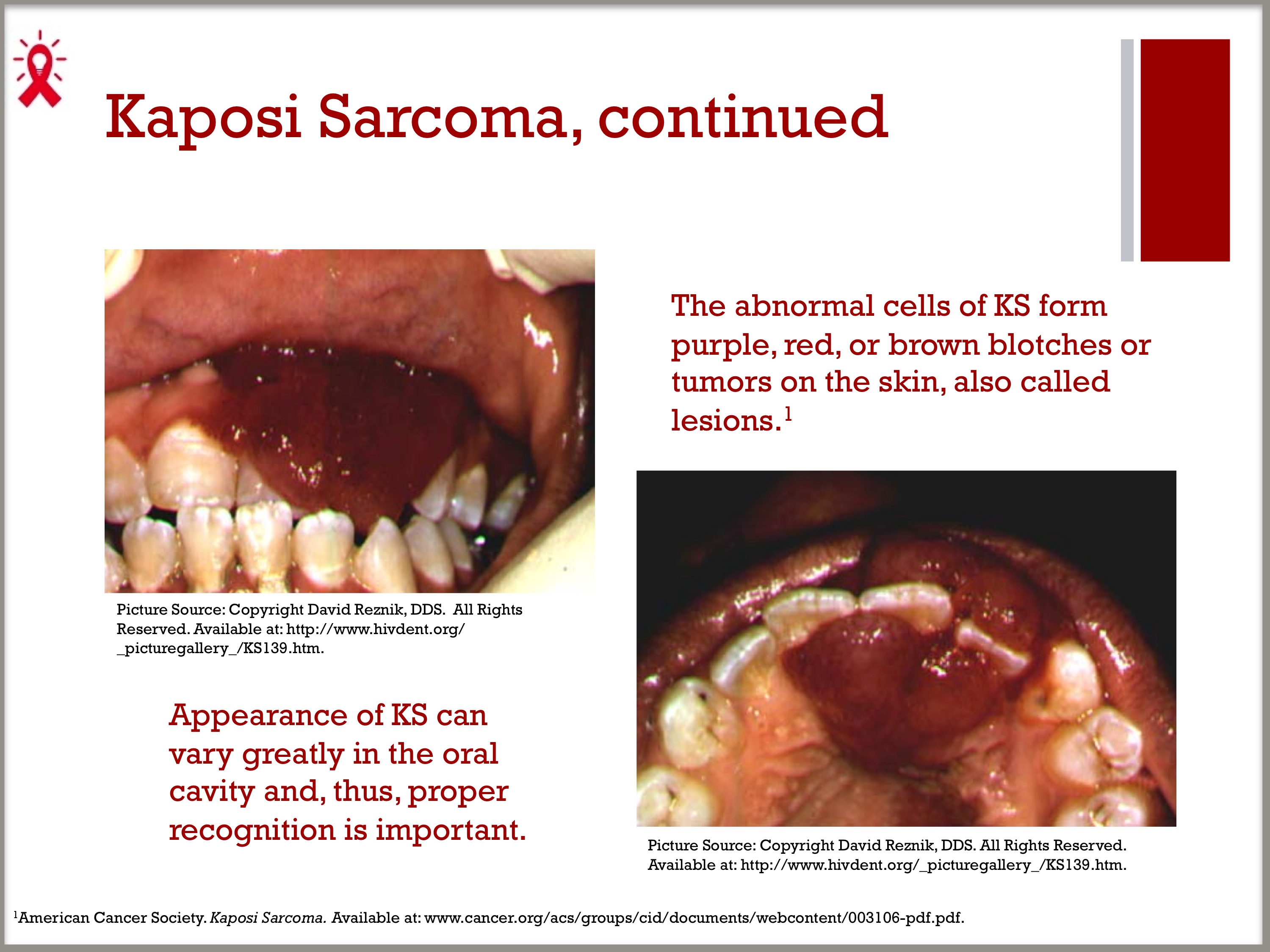
- Kaposi sarcoma (KS) is a cancer that develops from cells lining lymph or blood vessels. KS usually appears as tumors on the skin or on mucosal surfaces such as the oral cavity, but tumors can also develop in other parts of the body, such as in the lymph nodes or digestive tract. The abnormal cells of KS form purple, red, or brown blotches or tumors on the skin, also called lesions.1 That said, the appearance of KS can vary greatly in the oral cavity and, thus, proper recognition is important.
- Approximately one-third of PLWHA with AIDS-associated KS develop oral lesions. AIDS-associated KS is often much more aggressive than classic Kaposi sarcoma.2
- KS is considered an “AIDS-defining” illness, which means that when KS occurs in someone infected with HIV, that person officially has AIDS (and is not just HIV-positive).3
1. American Cancer Society. Kaposi Sarcoma.
2. Memorial Sloan-Kettering Cancer Center. About Kaposi Sarcoma.
3. American Cancer Society. Kaposi Sarcoma.
SLIDE 8: Other STDs and their Impact on Oral Health
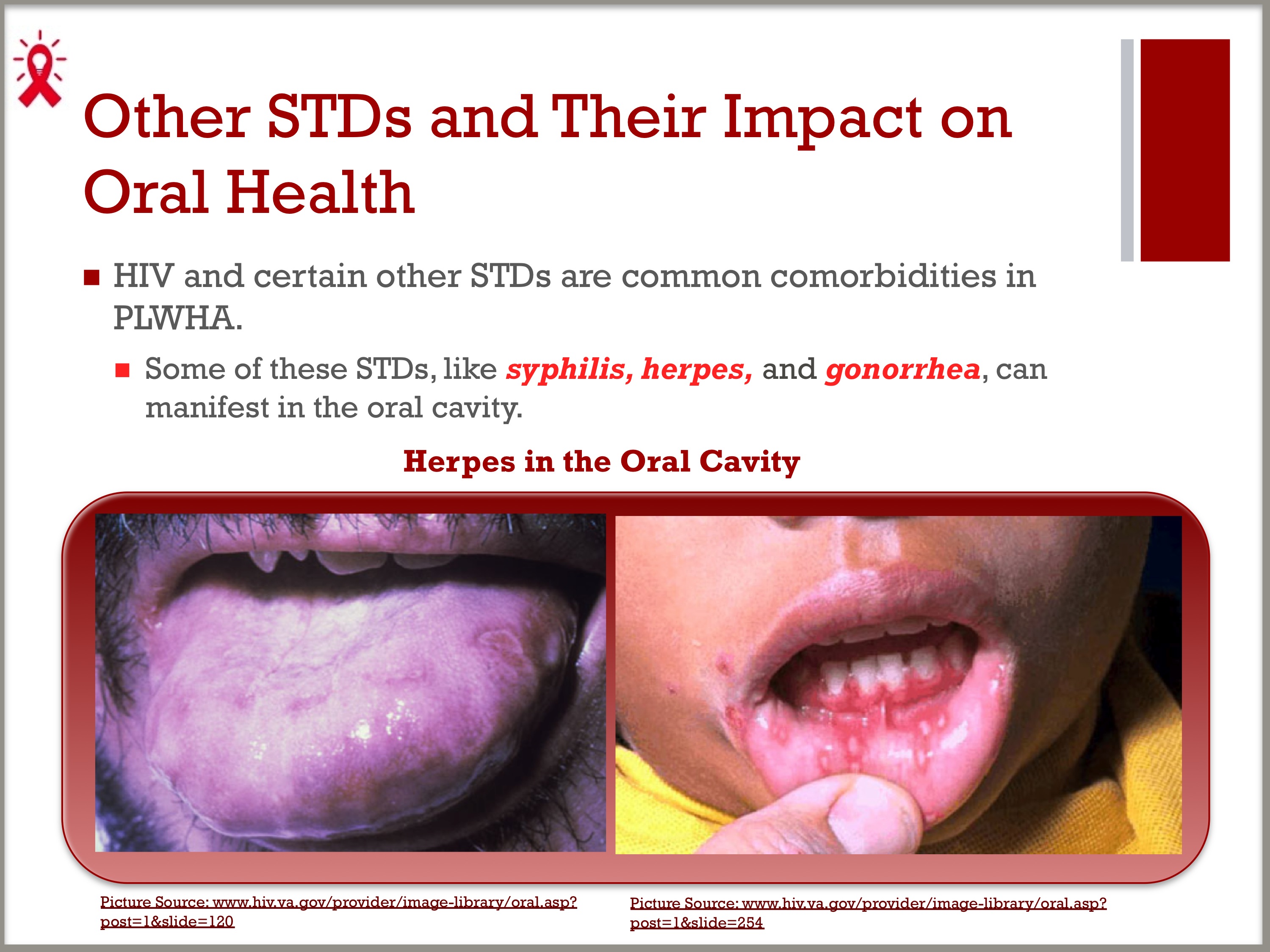
- HIV and certain other STDs are common comorbidities in PLWHA.
- Some of these STDs, like syphilis, herpes, and gonorrhea, can manifest in the oral cavity.
SLIDE 9: HIV and Syphilis
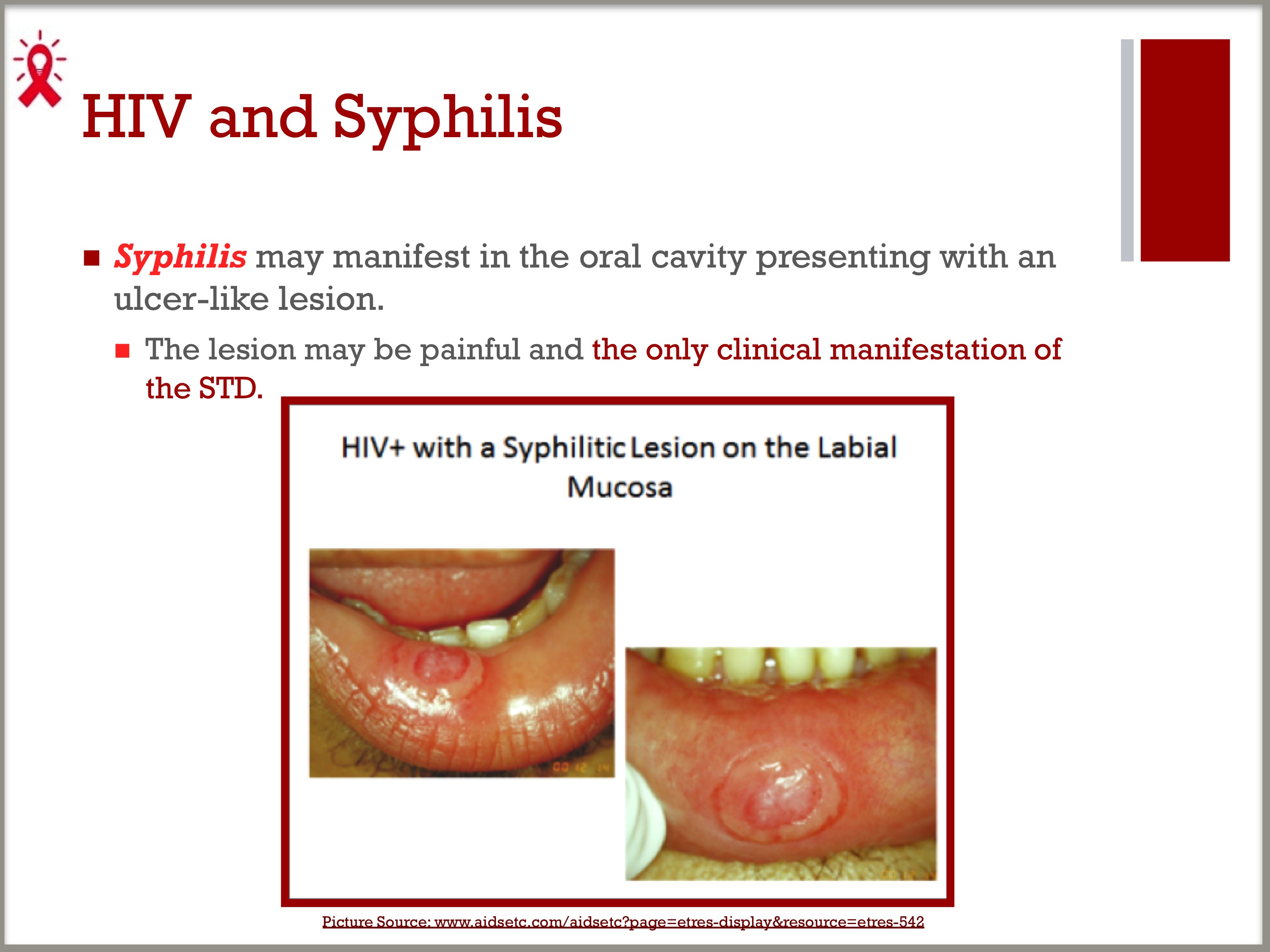
- Syphilis may manifest in the oral cavity presenting with an ulcer-like lesion.
- The lesion may be painful and the only clinical manifestation of the STD.
SLIDE 10: HIV and Oral Gonorrhea
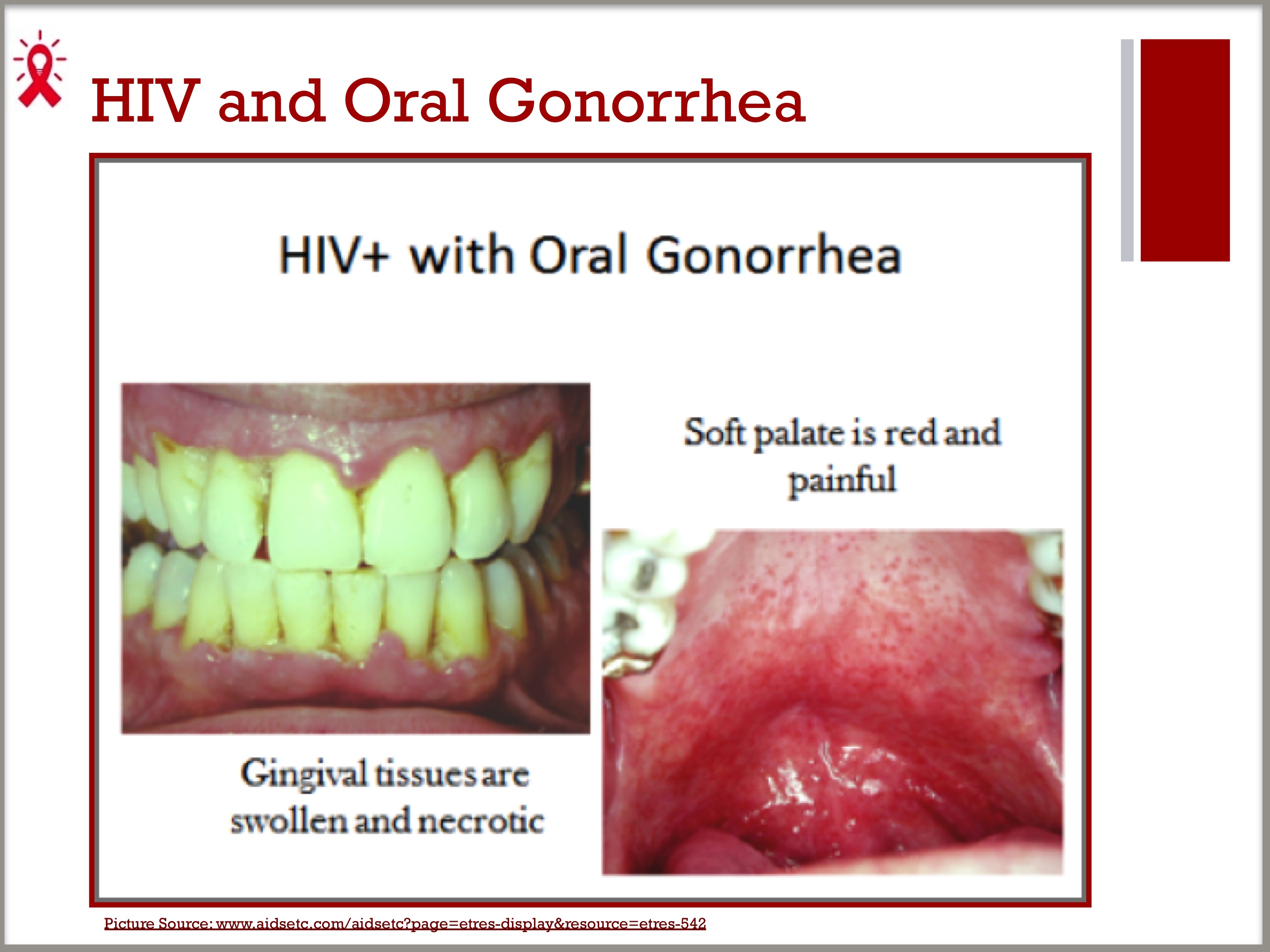
- The following patient presented with severe gingival pain and a sore throat. He had oral sex with his partner a few days before. He found out later that his partner had genital gonorrhea.
SLIDE 11: Oral Health Exam Training Video for Clinical Staff
Video
- Oral Health History and Examination featuring Carol Stewart, DDS, MS, MS, Dental Director of the Florida/Caribbean AETC and Professor and Director of the Division of Oral Diagnostic Sciences, Department of Oral and Maxillofacial Surgery and Diagnostic Sciences at the University of Florida College of Dentistry
- Explain to the class that this video presentation provides instruction on performing both external and intraoral exams.
- Have the class watch the video (approximately 12 minutes in length).
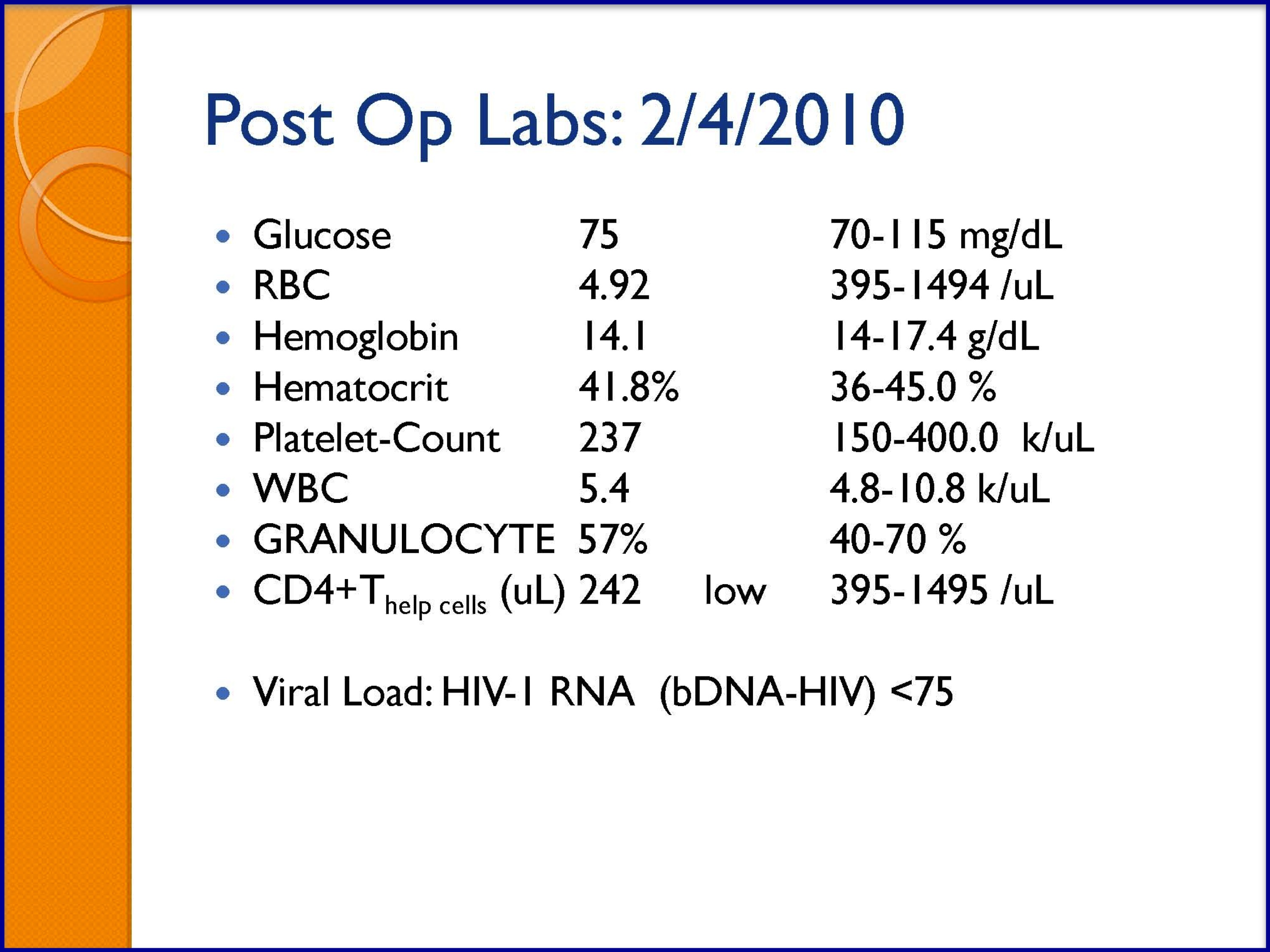
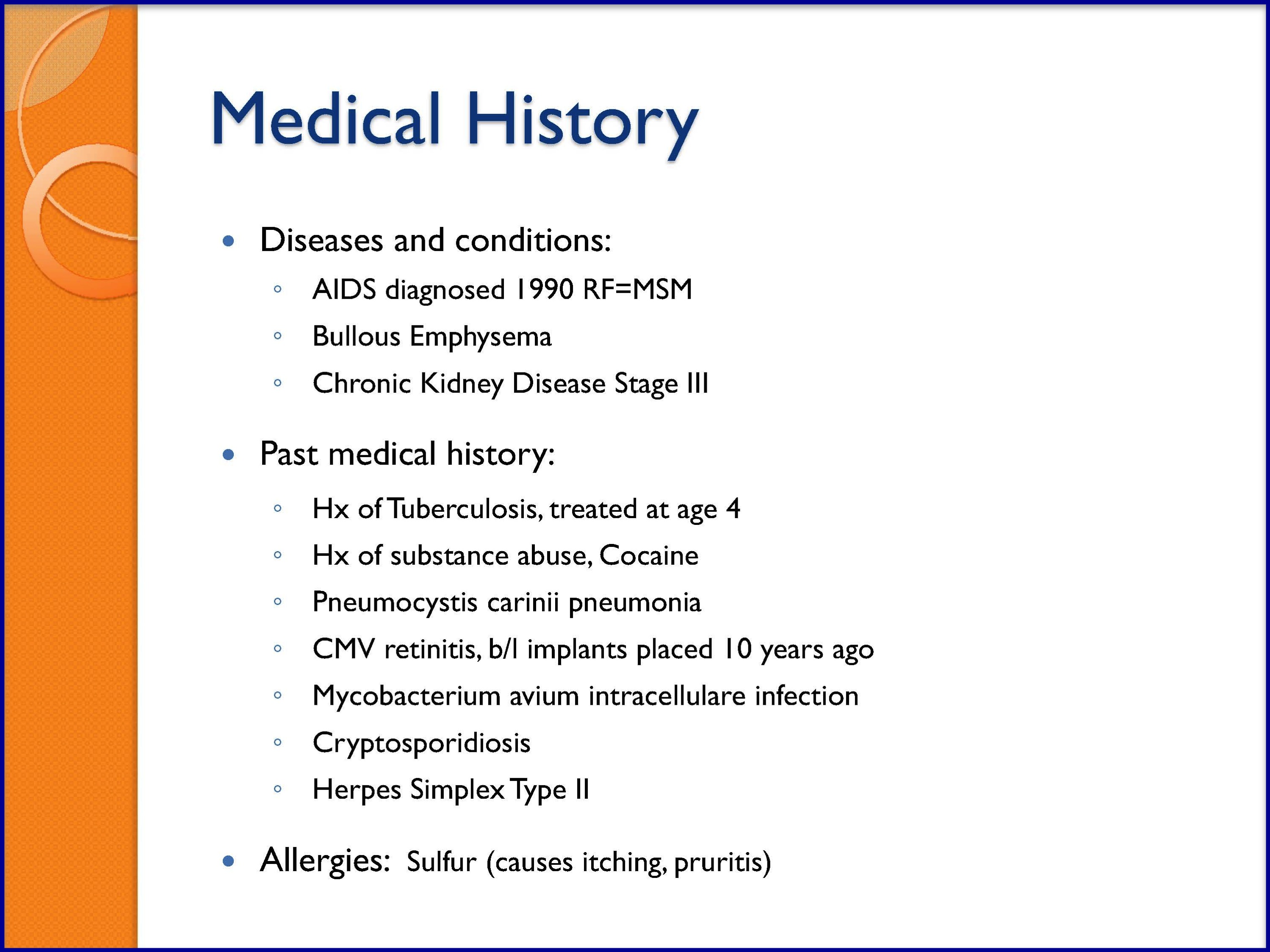
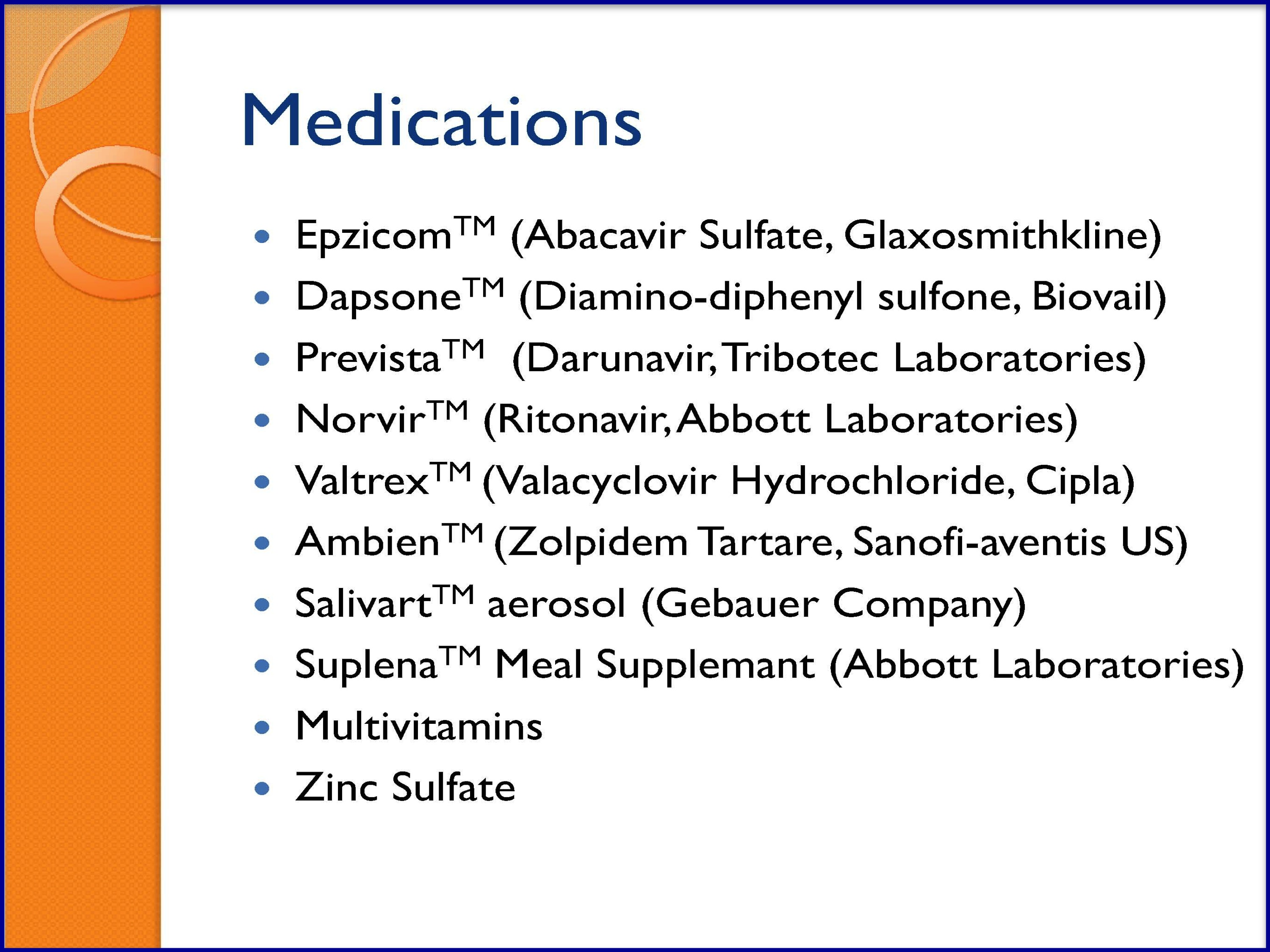
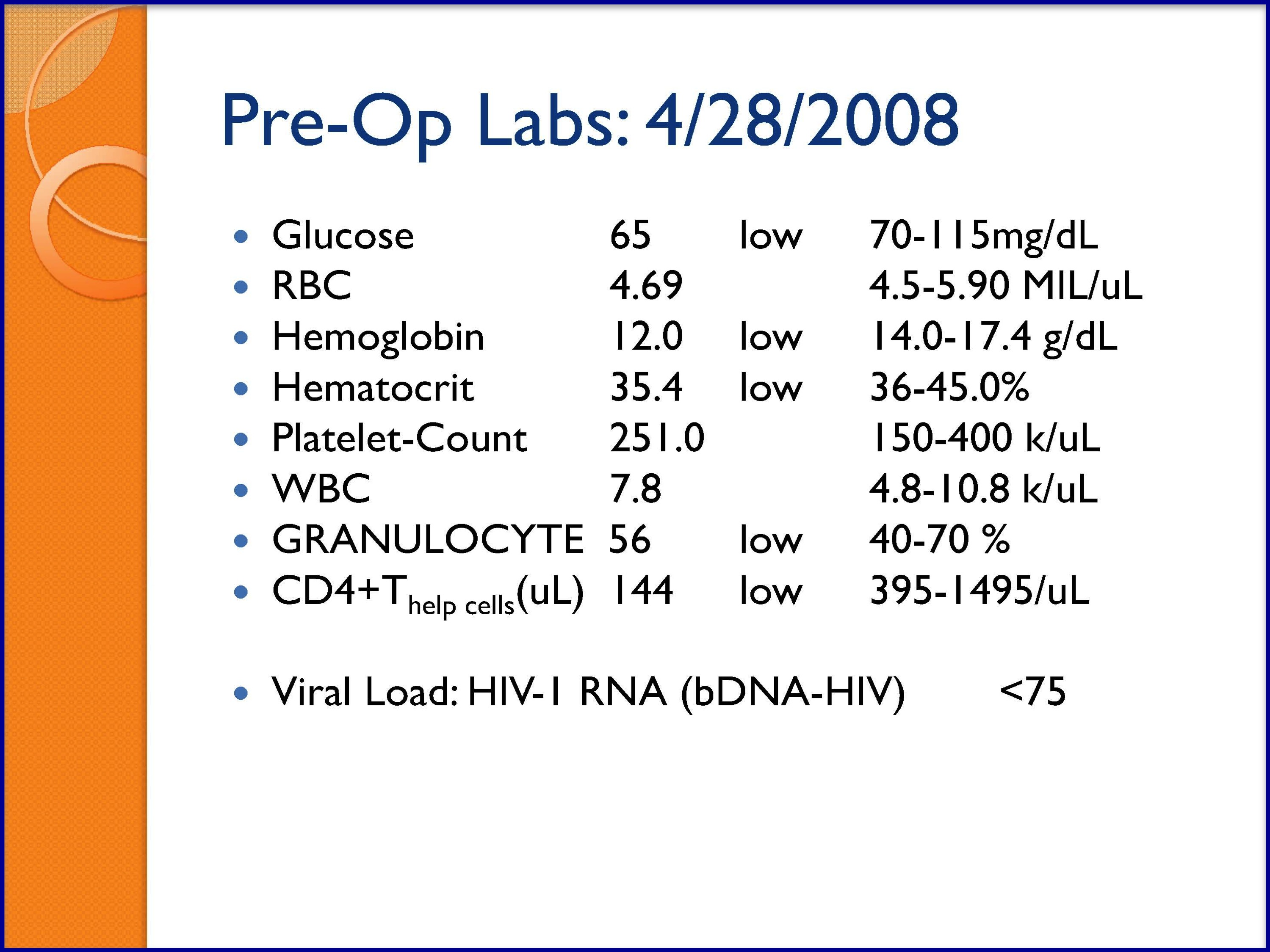
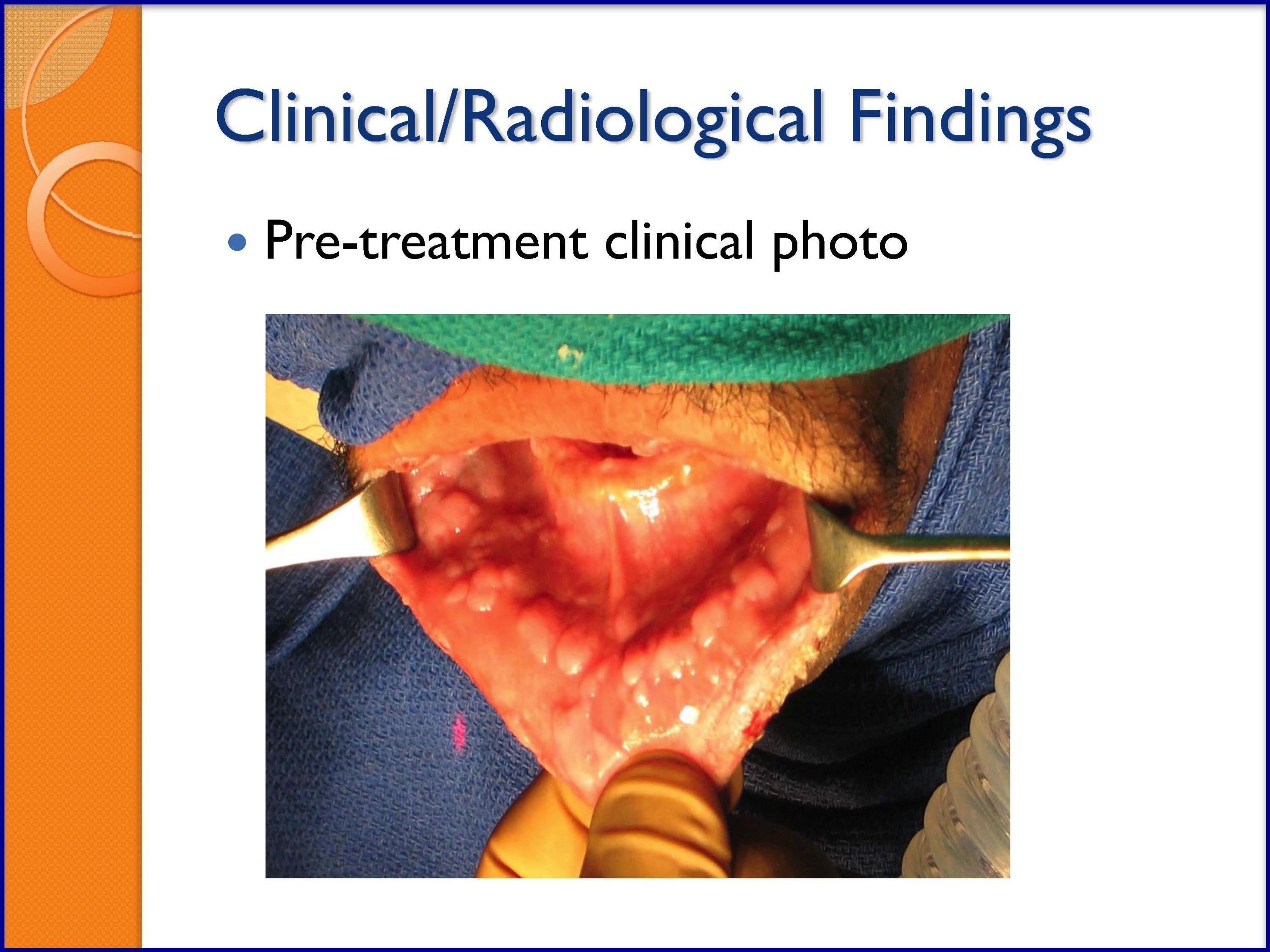
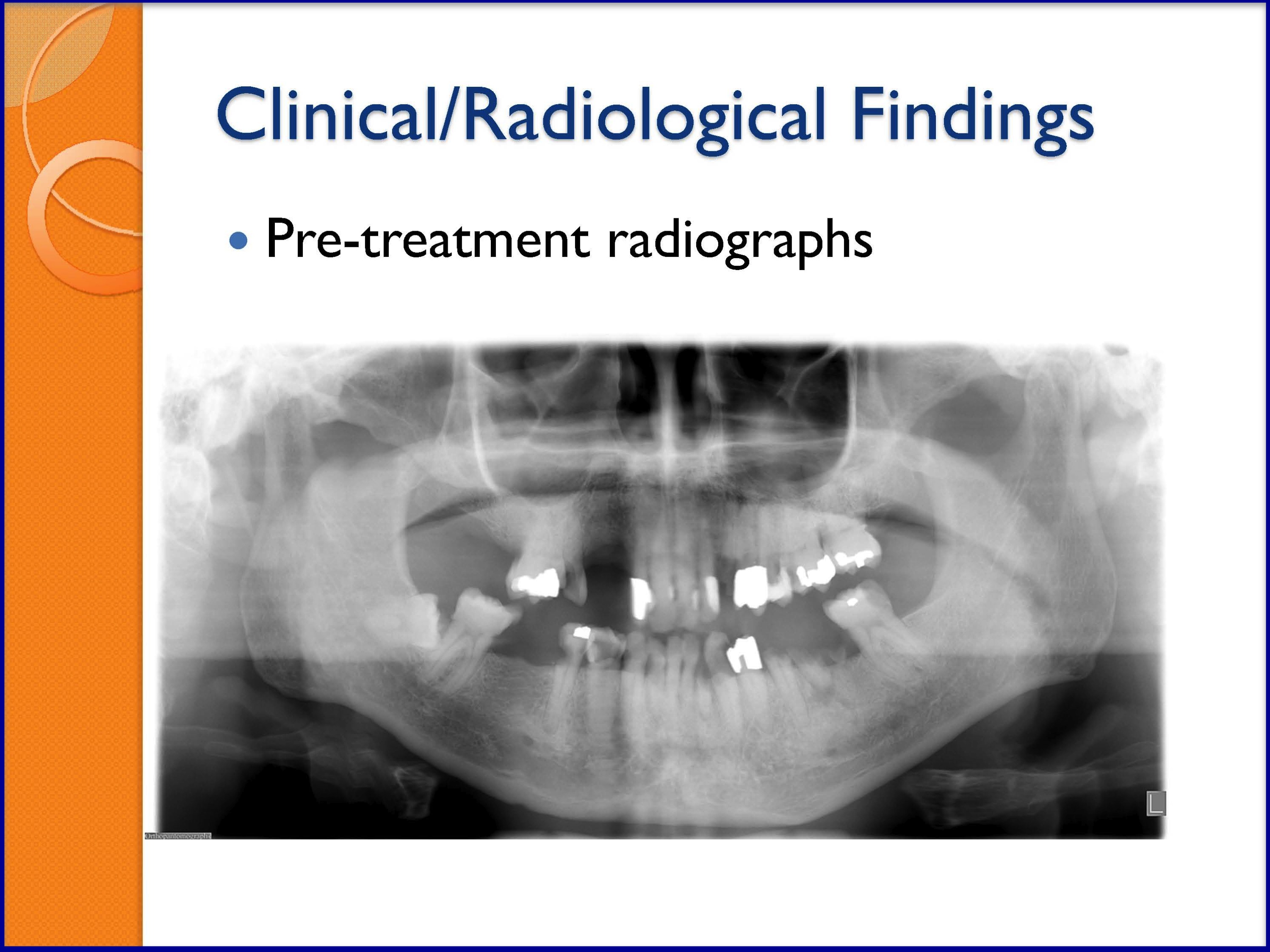
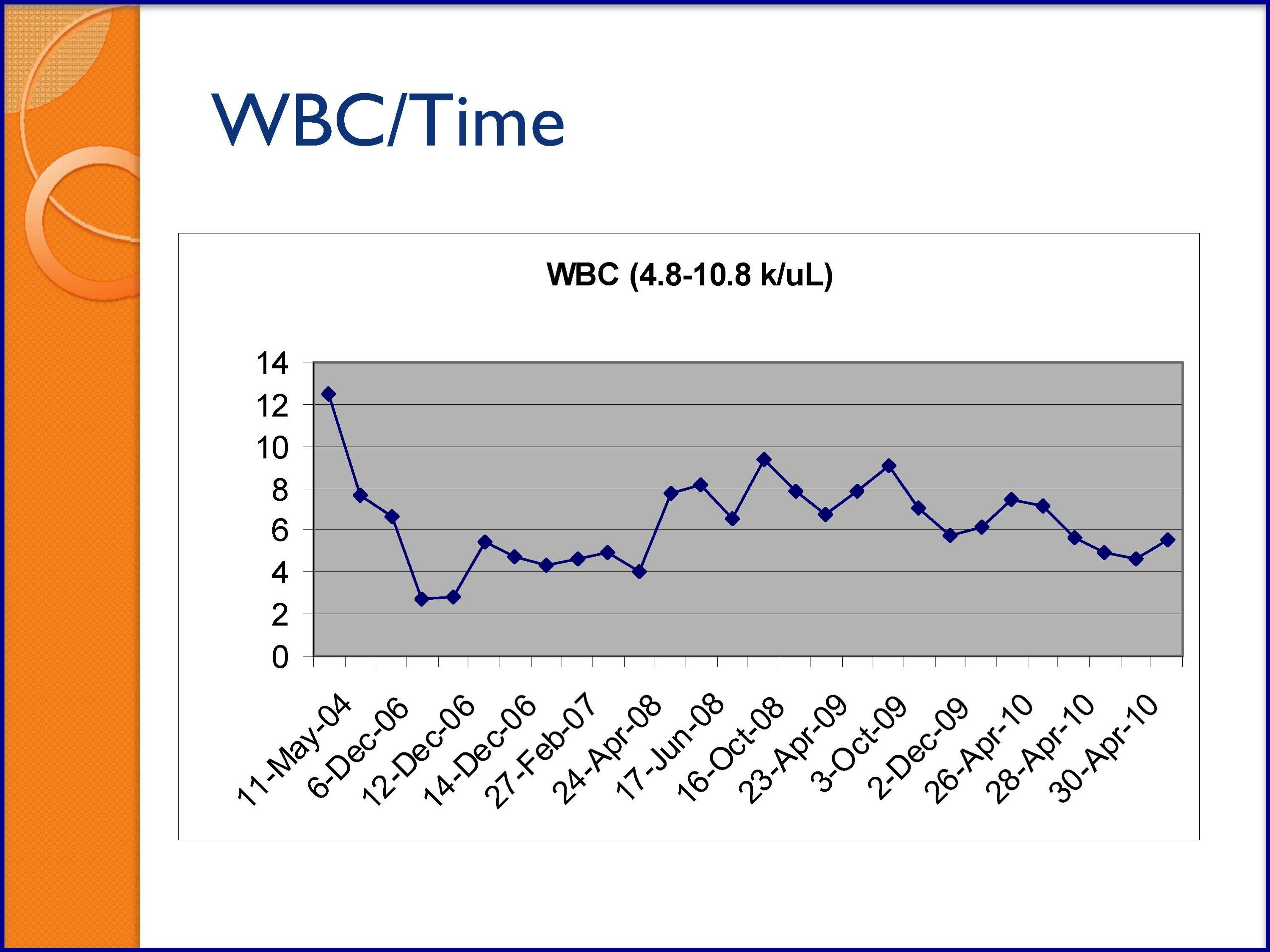
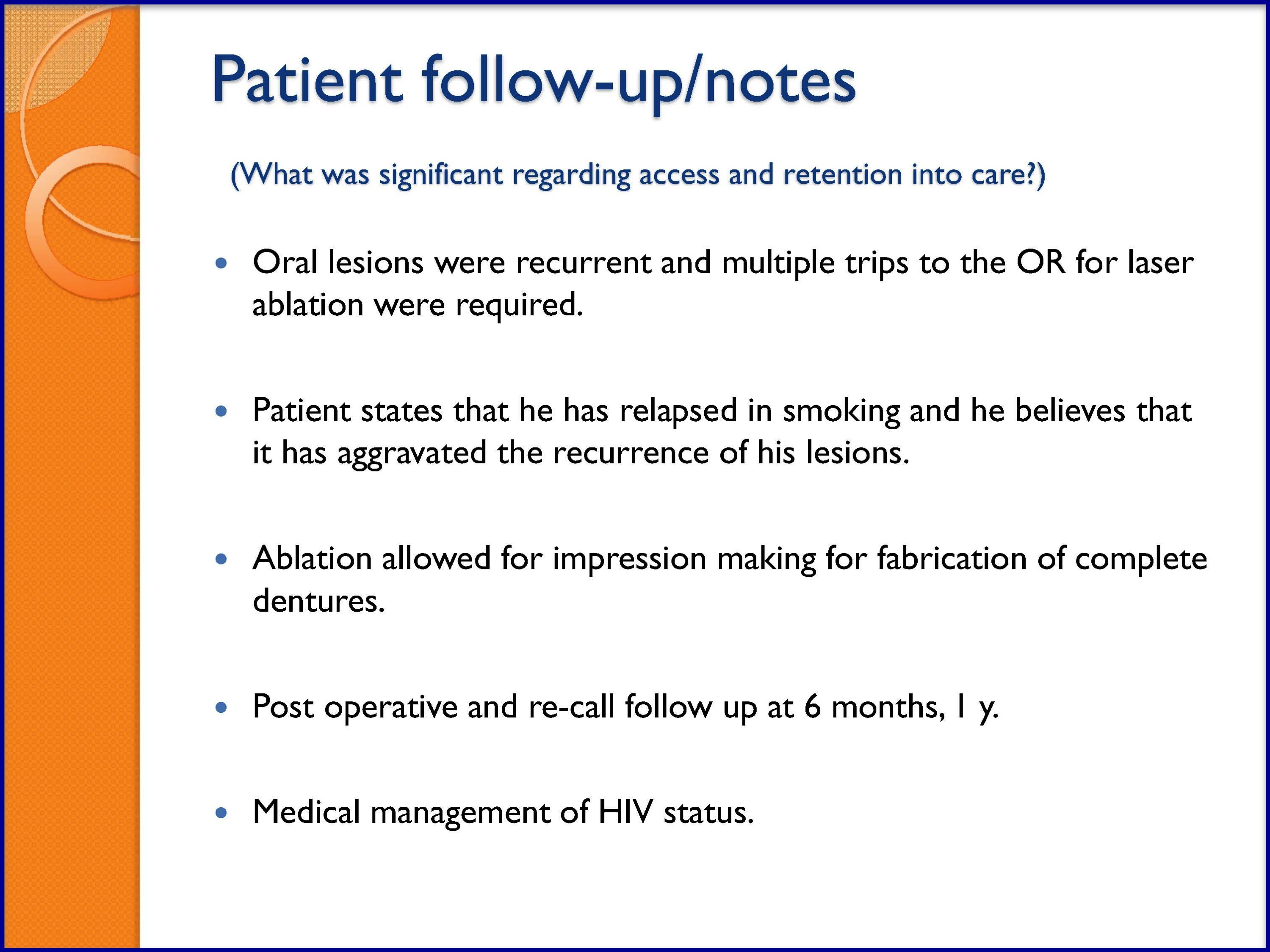
SLIDES 12–58: Case Studies: Florid HPV and Kaposi Sarcoma
The following cases studies were adapted from case studies prepared by J. Kazimiroff, BS, DDS, MS FAGD, FACD, CertEd; and K. Alvarado, DMD. Both Dr. Kazimiroff and Dr. Alvarado are from the Montefiore Medical Center at The University Hospital of Albert Einstein College of Medicine of Yeshiva University.
GROUP ACTIVITY
Case Study Discussion
- Pass out handouts of the case studies below to each participant.
- Kaposi Sarcoma
- Florid Human Papillomavirus (HPV) Oral Lesions
- Break the class into small groups of 3 to 4 people and discuss the presentation and treatment options for the case studies (15 minutes total).
After discussion, assign one person to deliver each group’s assessment of the cases with the class.
SLIDES 12-17
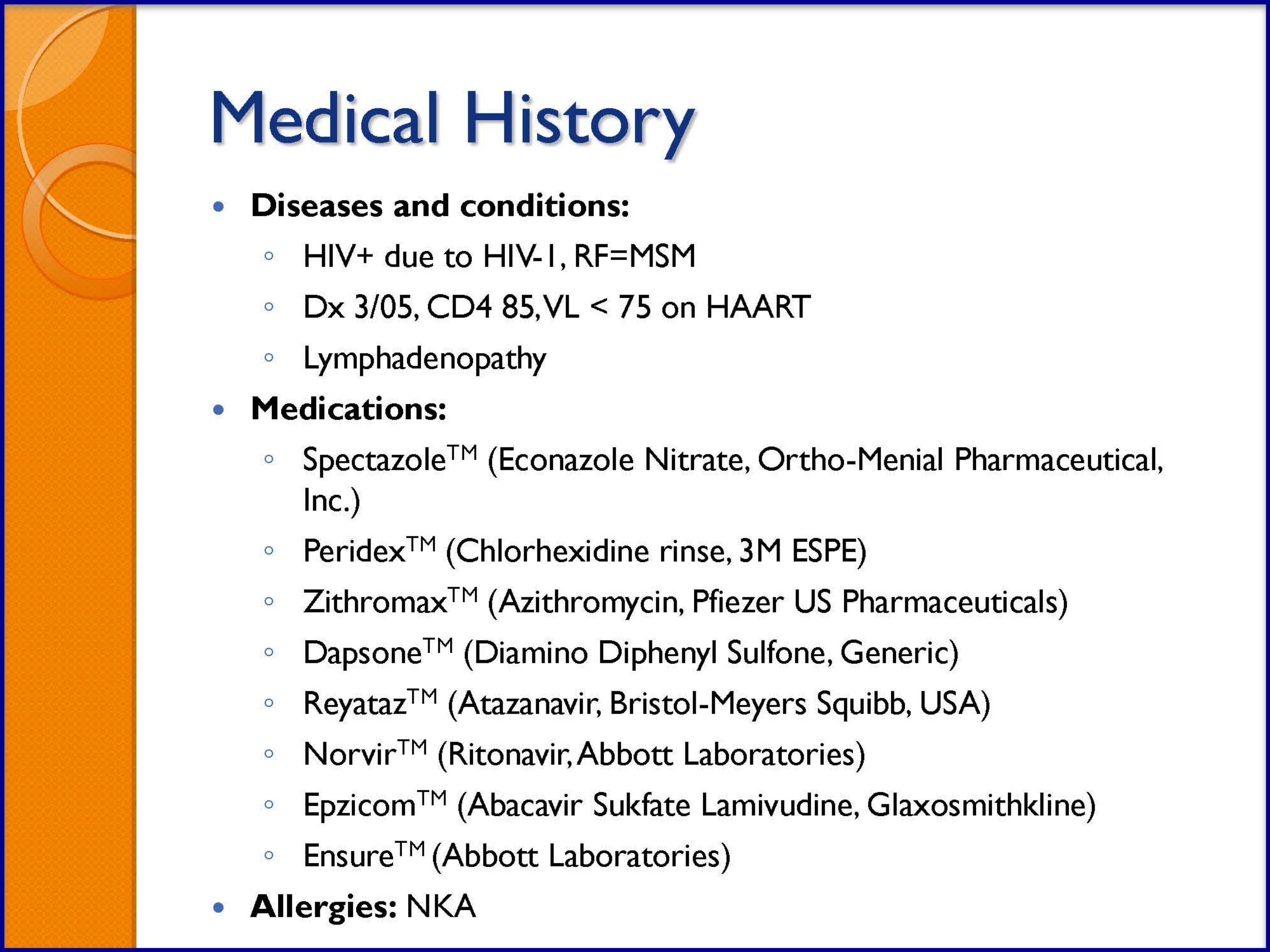
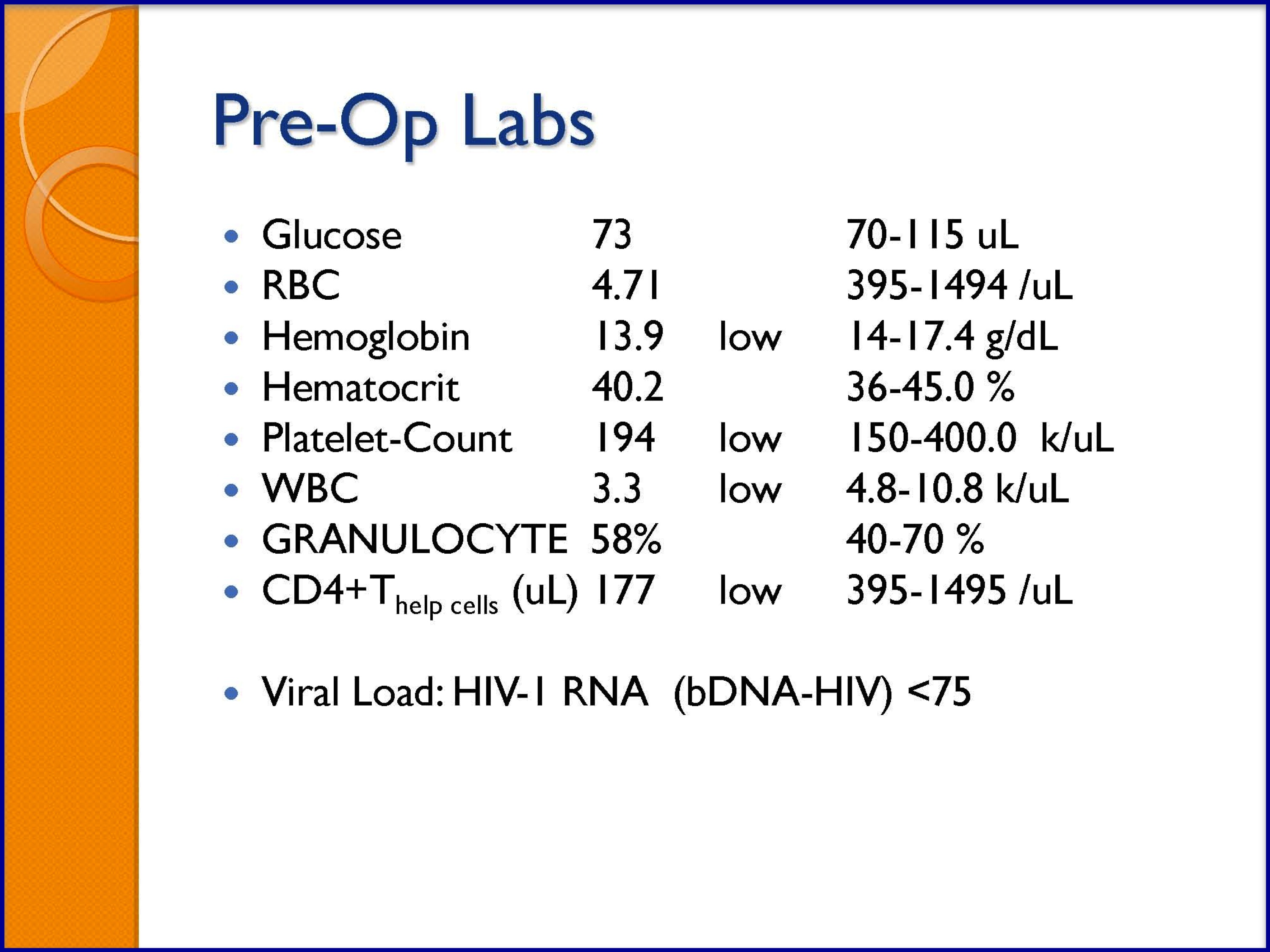
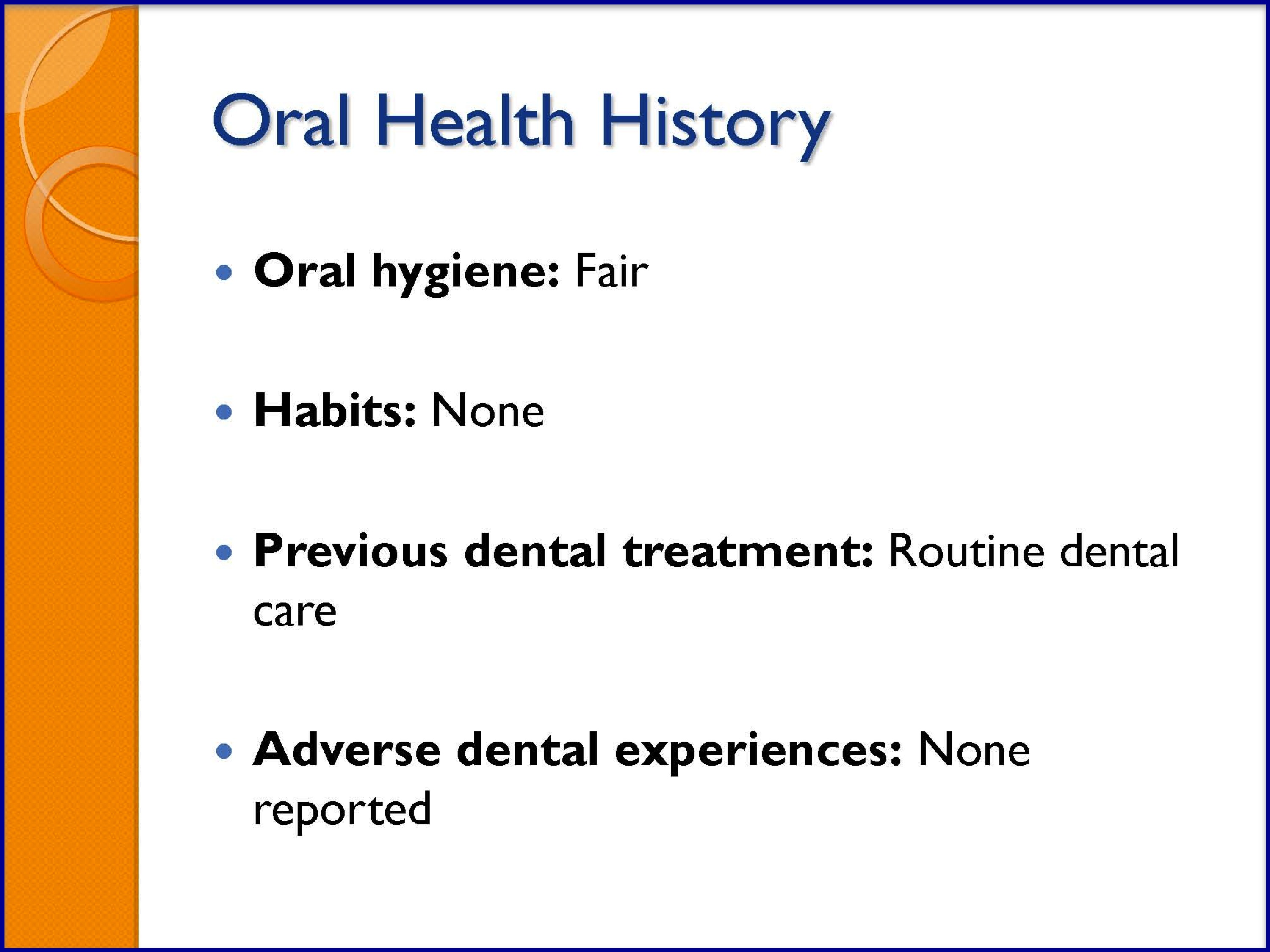
SLIDES 18-23
SLIDES 24-29


SLIDES 30-35
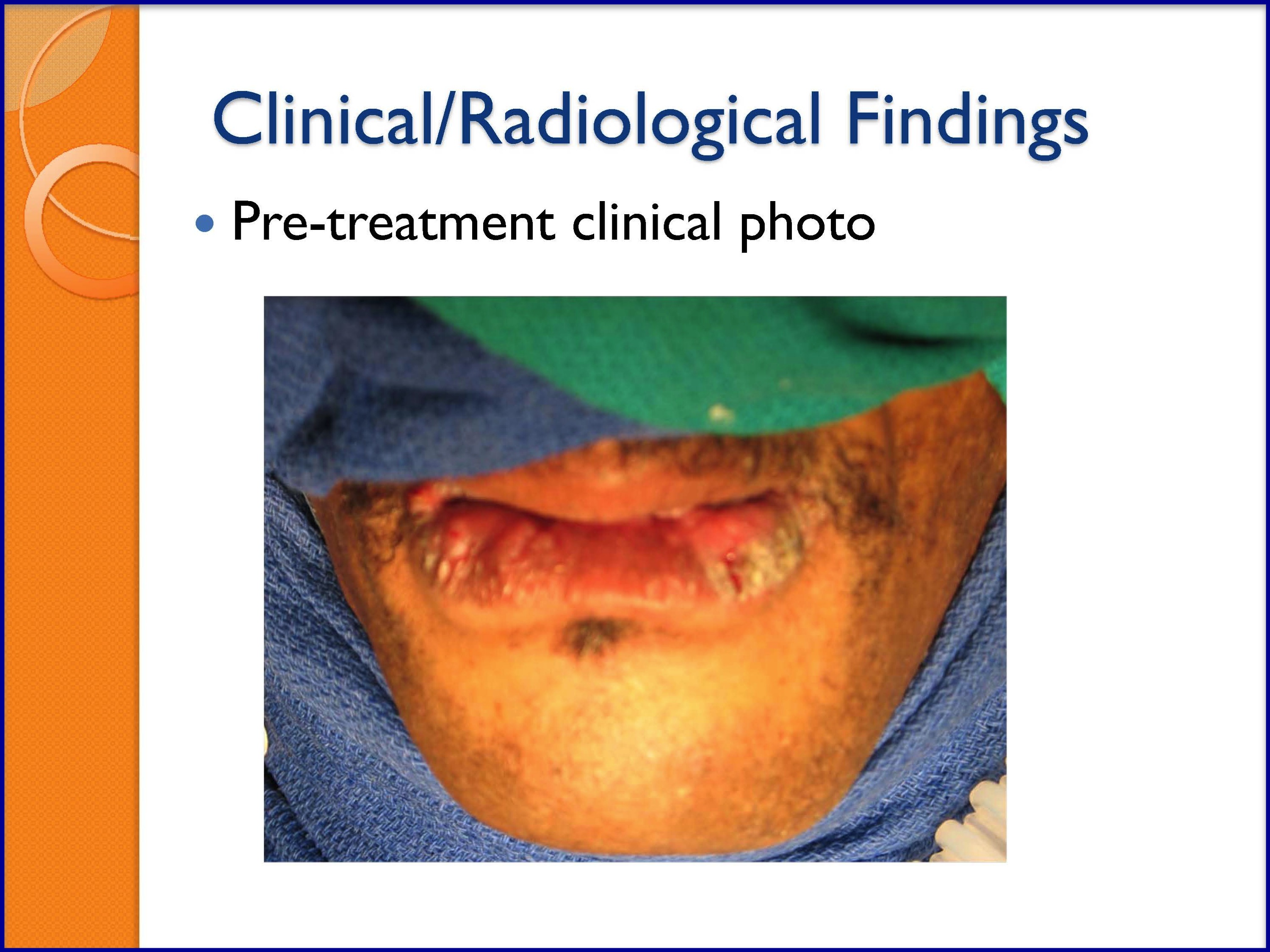
SLIDES 36-41
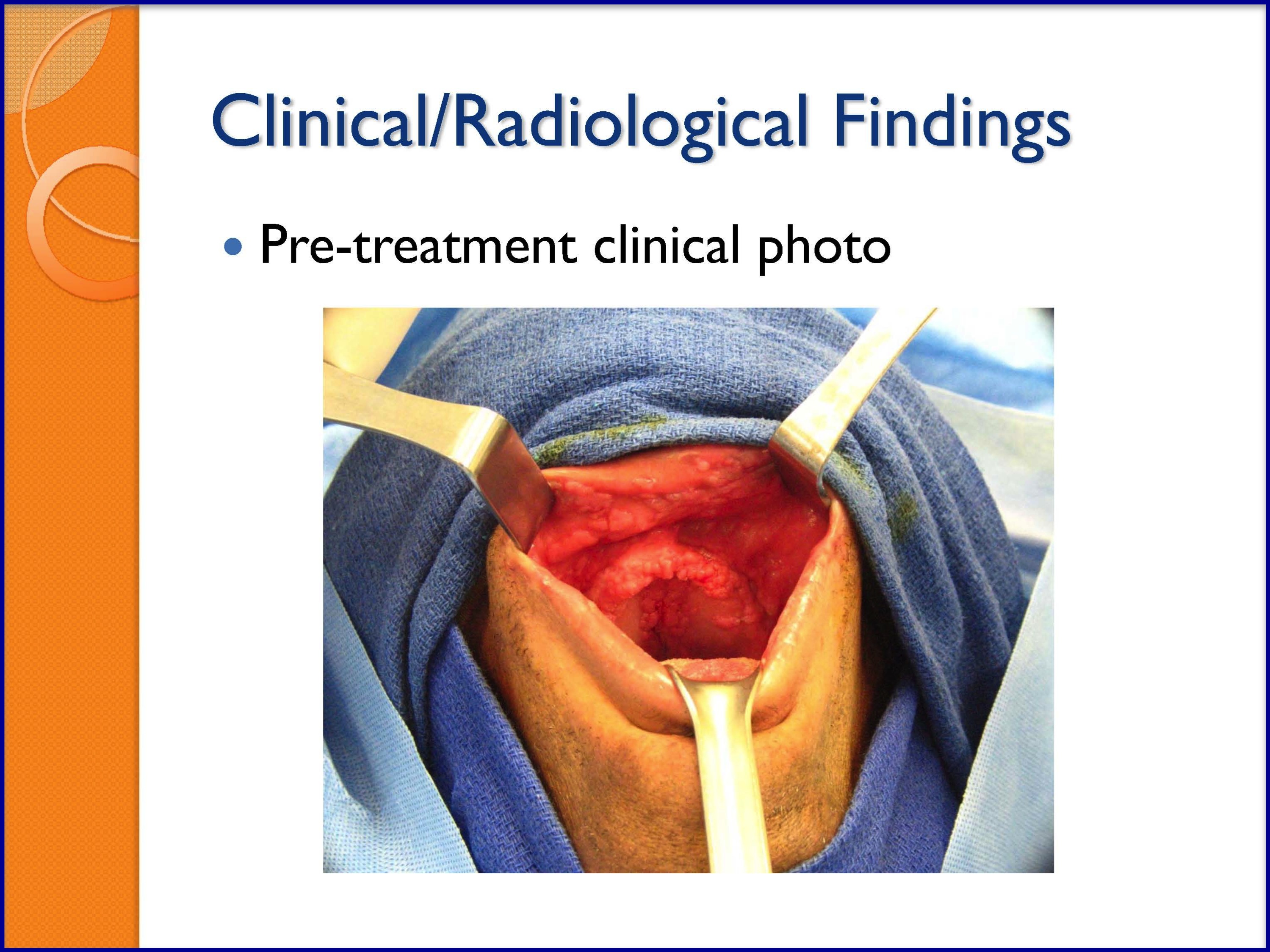

SLIDES 42-47

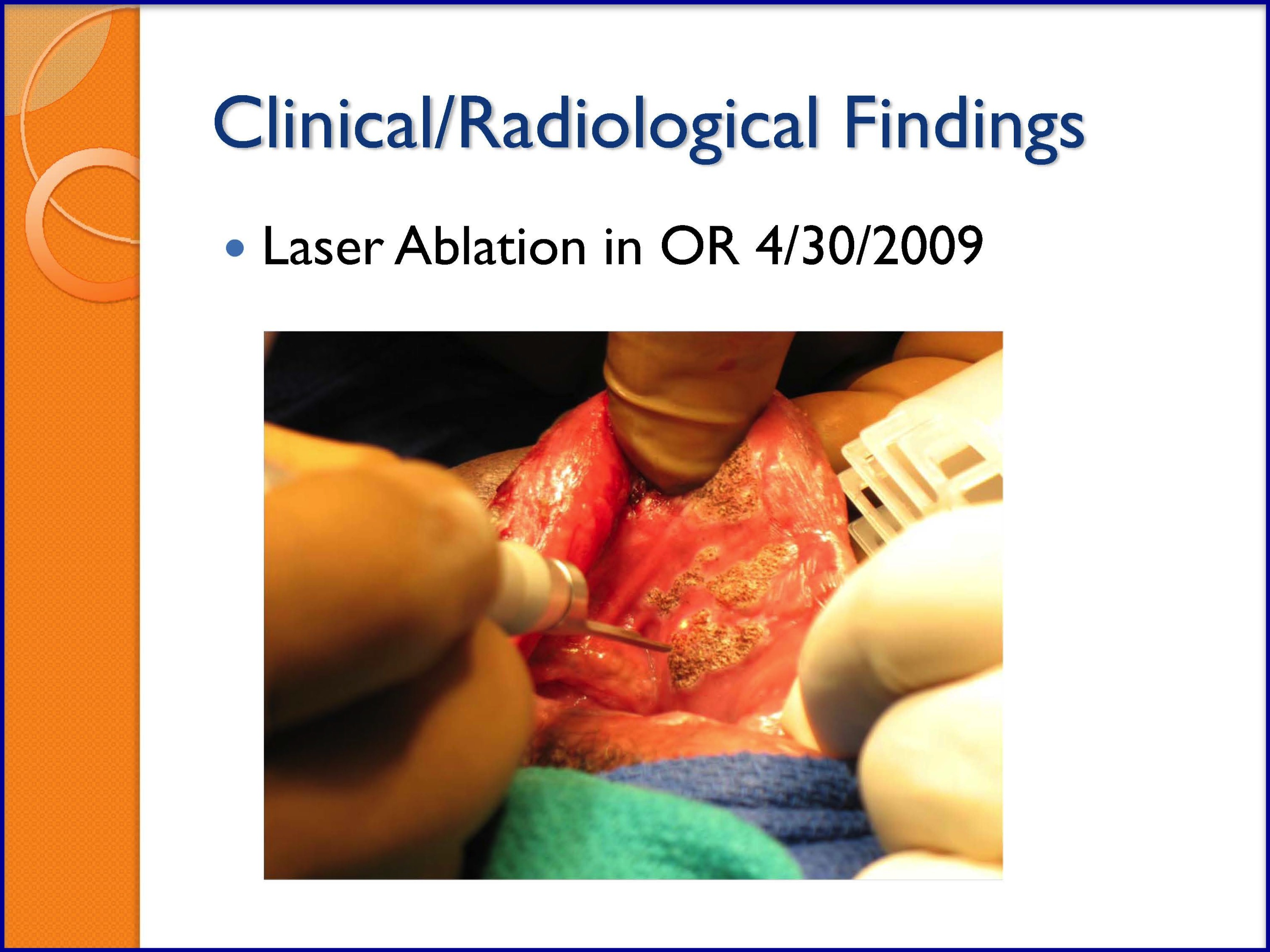
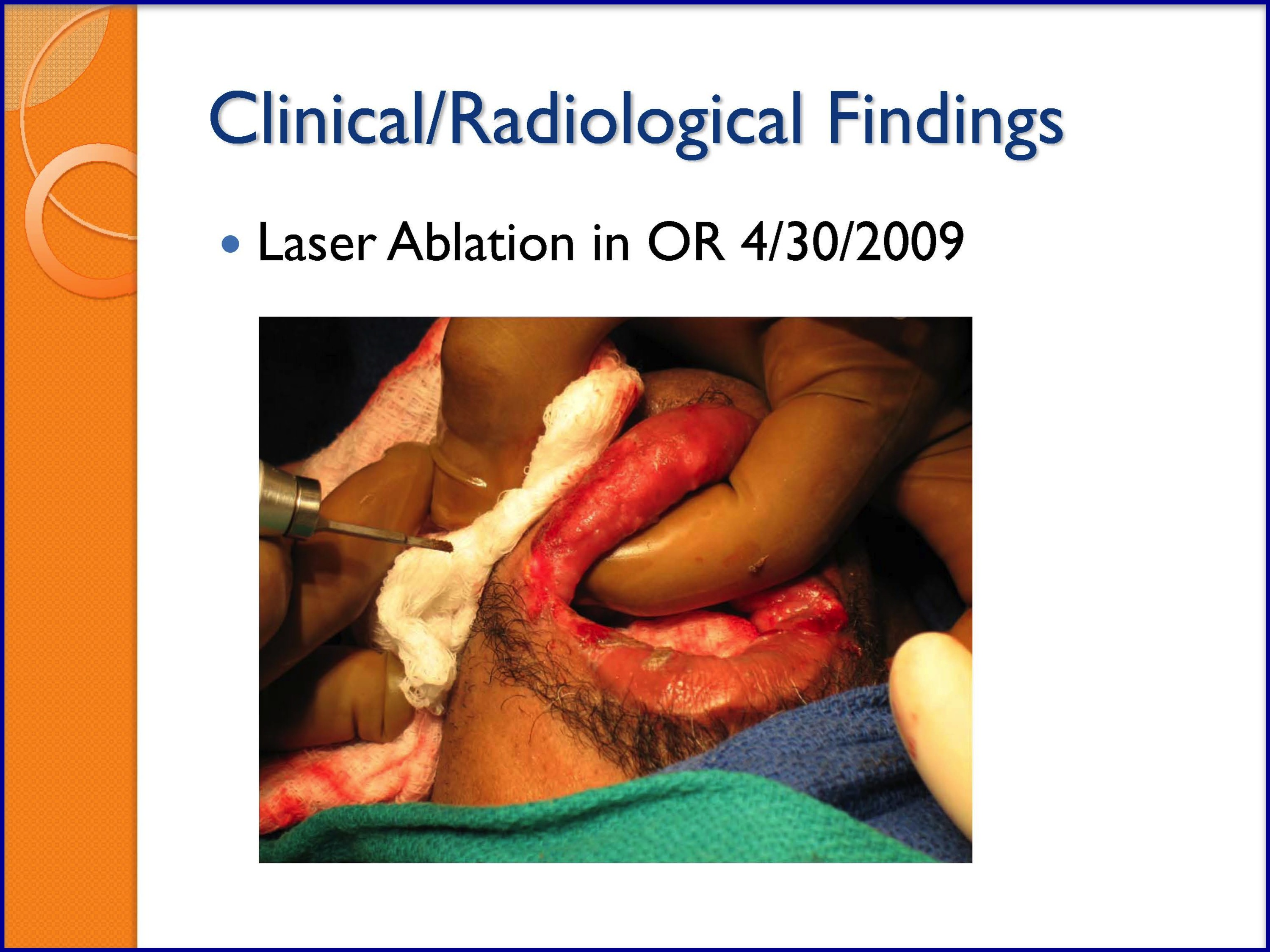
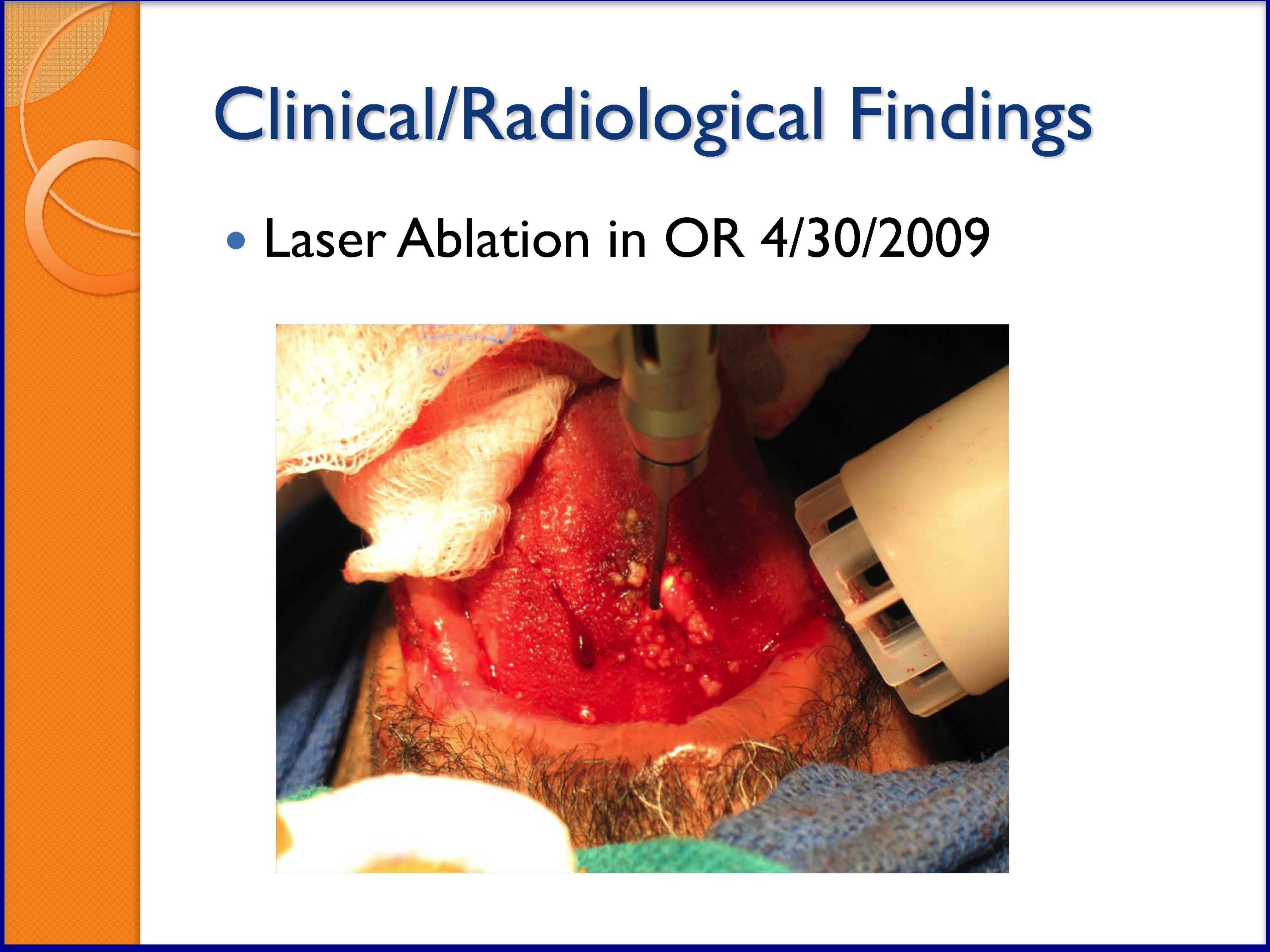
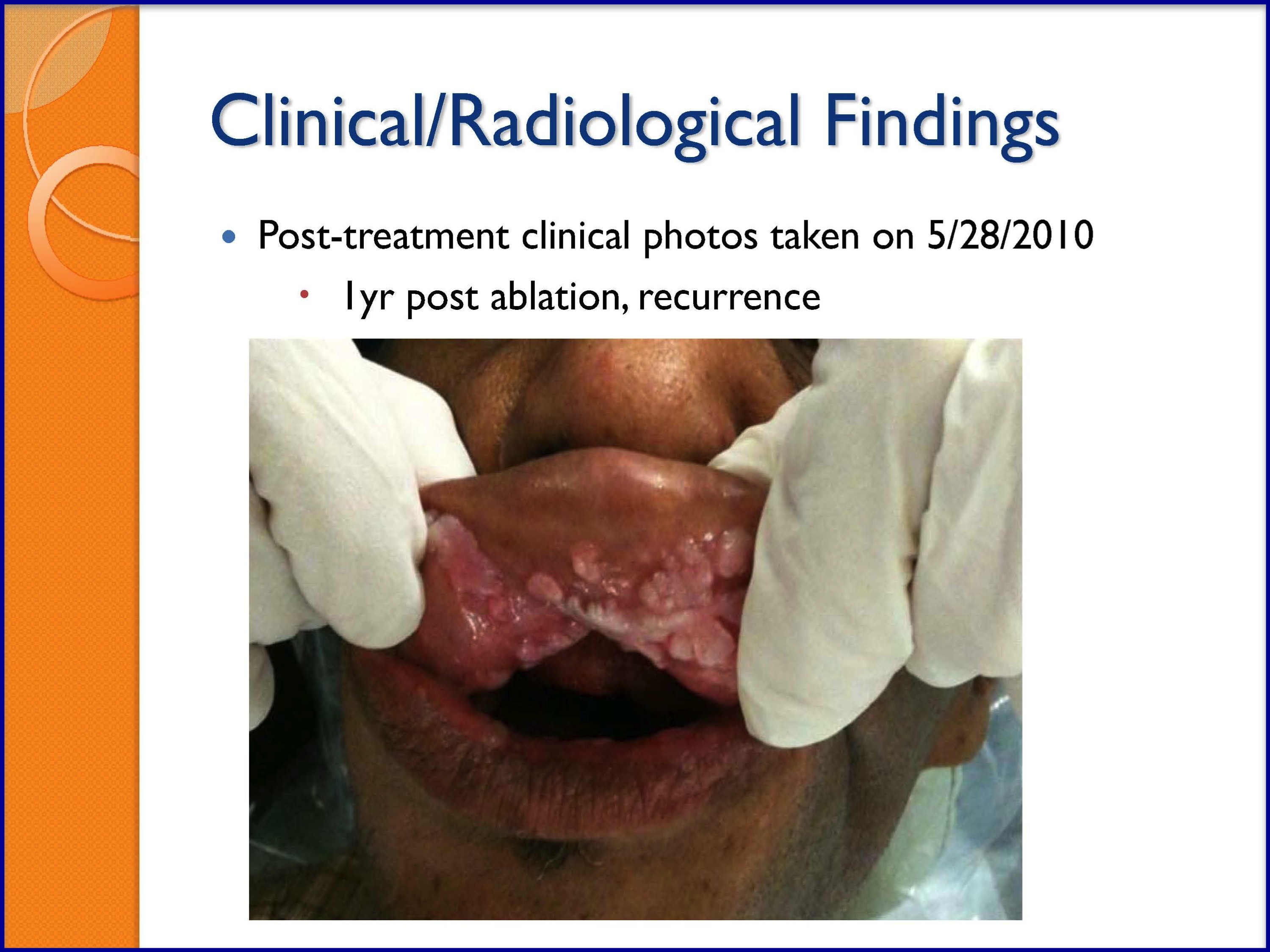
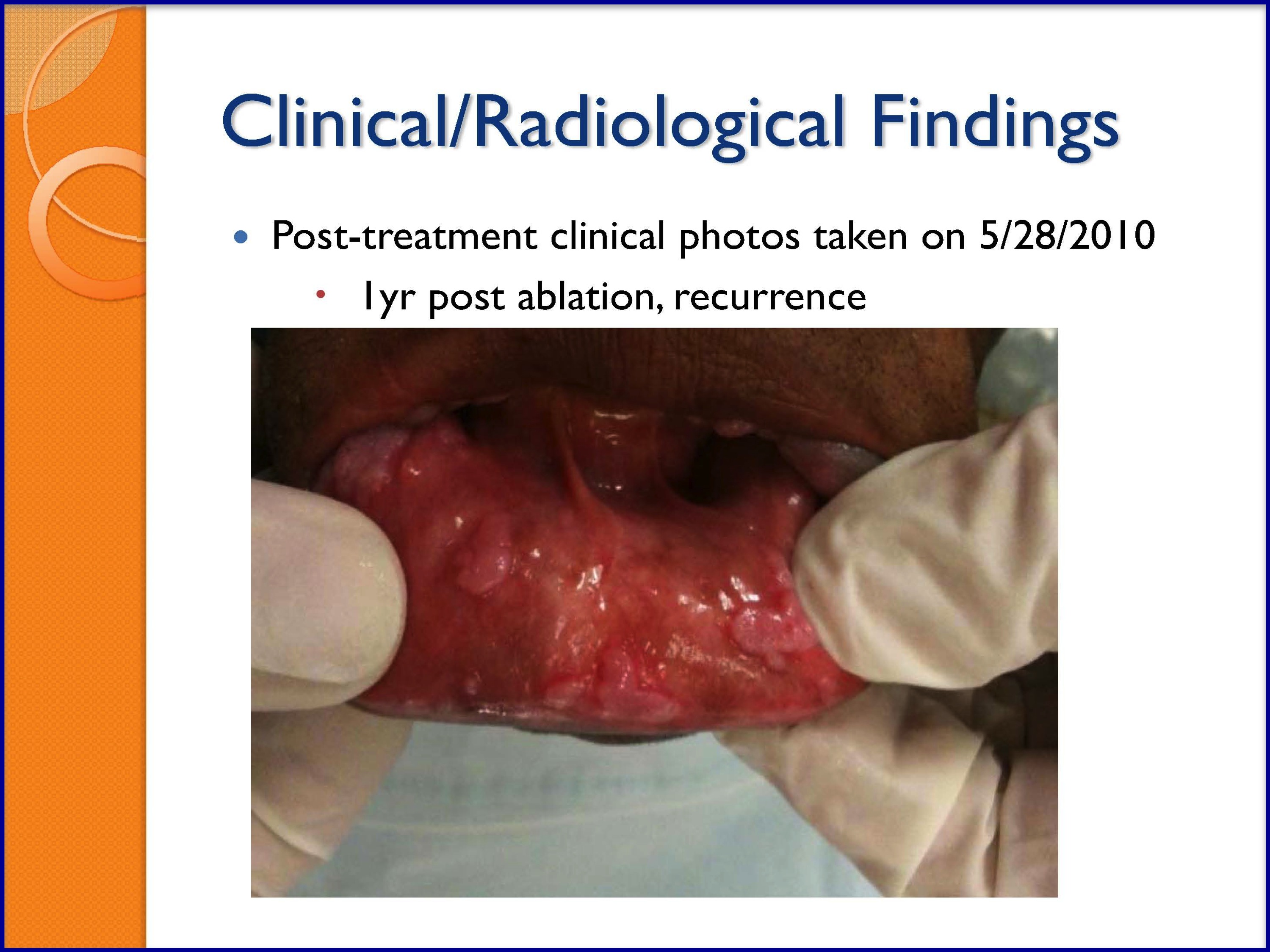
SLIDES 48-53
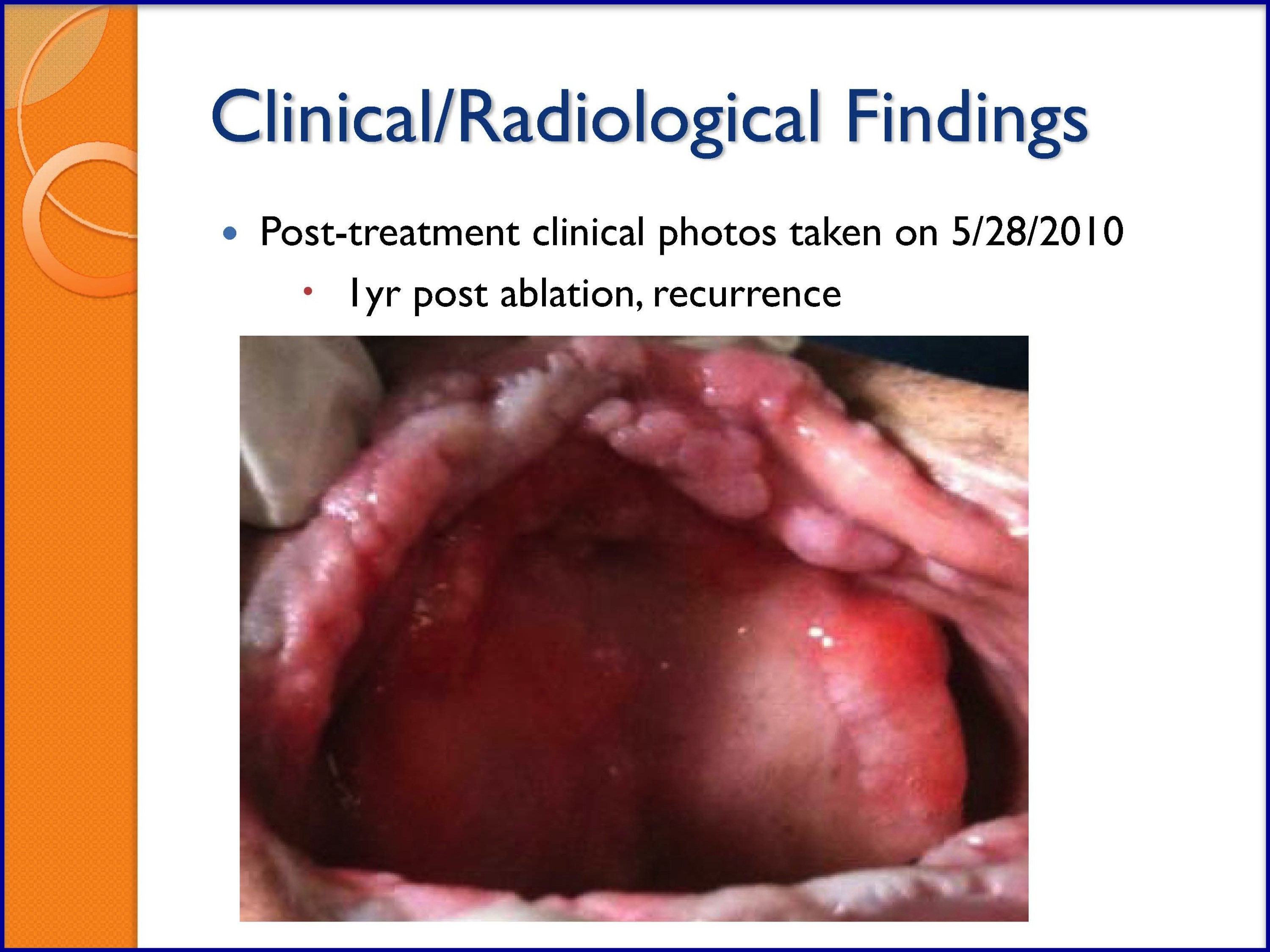
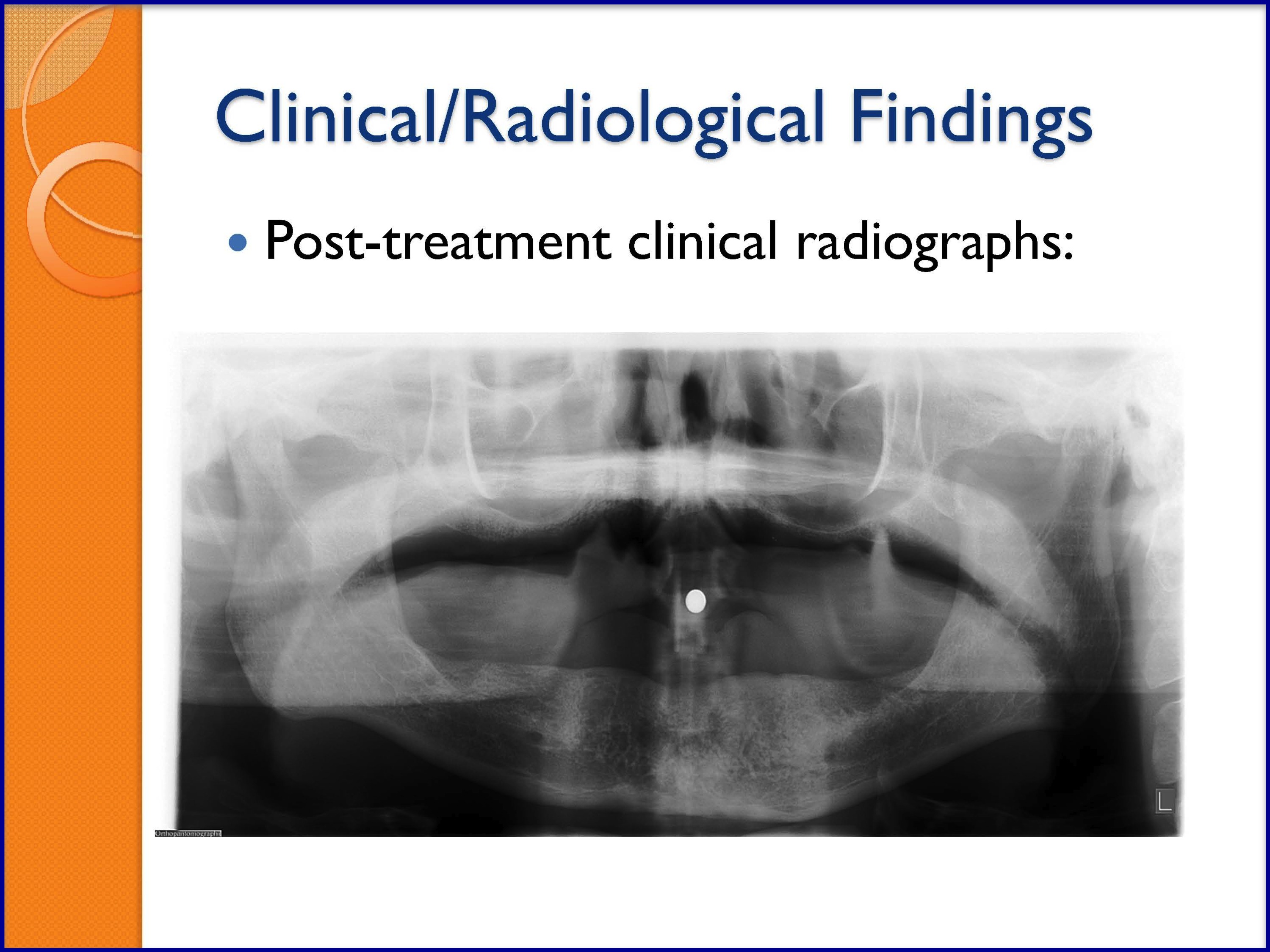
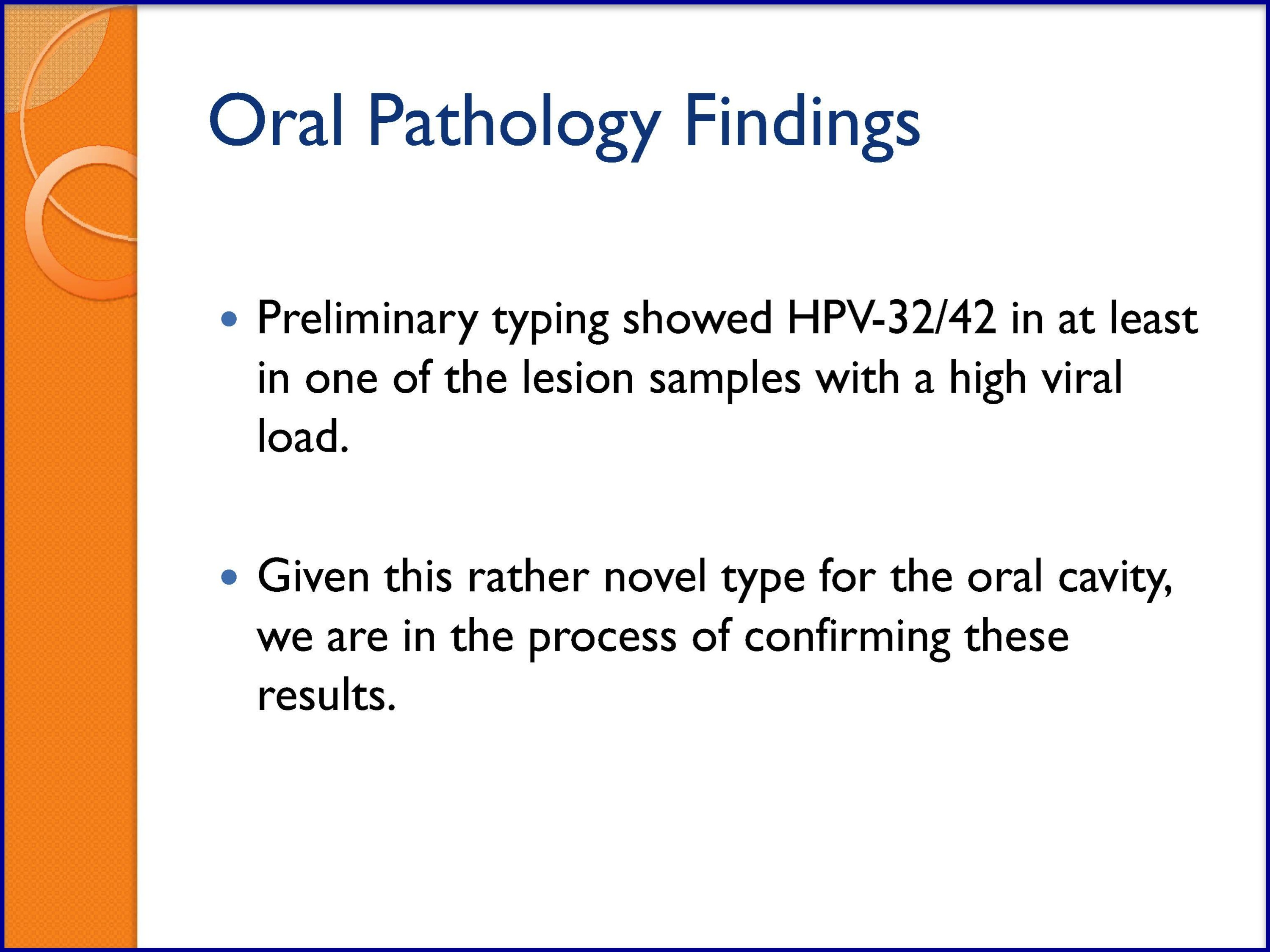
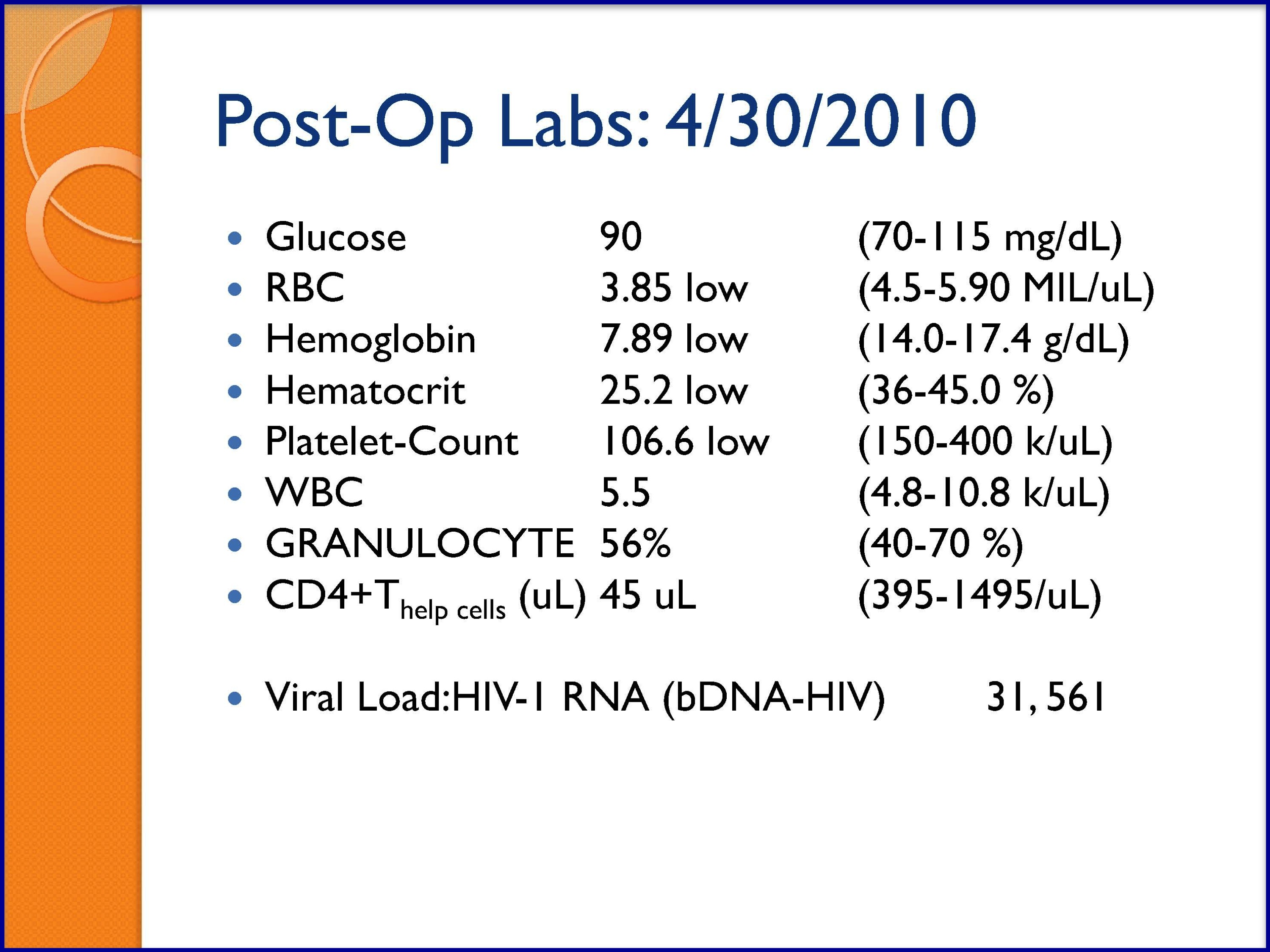
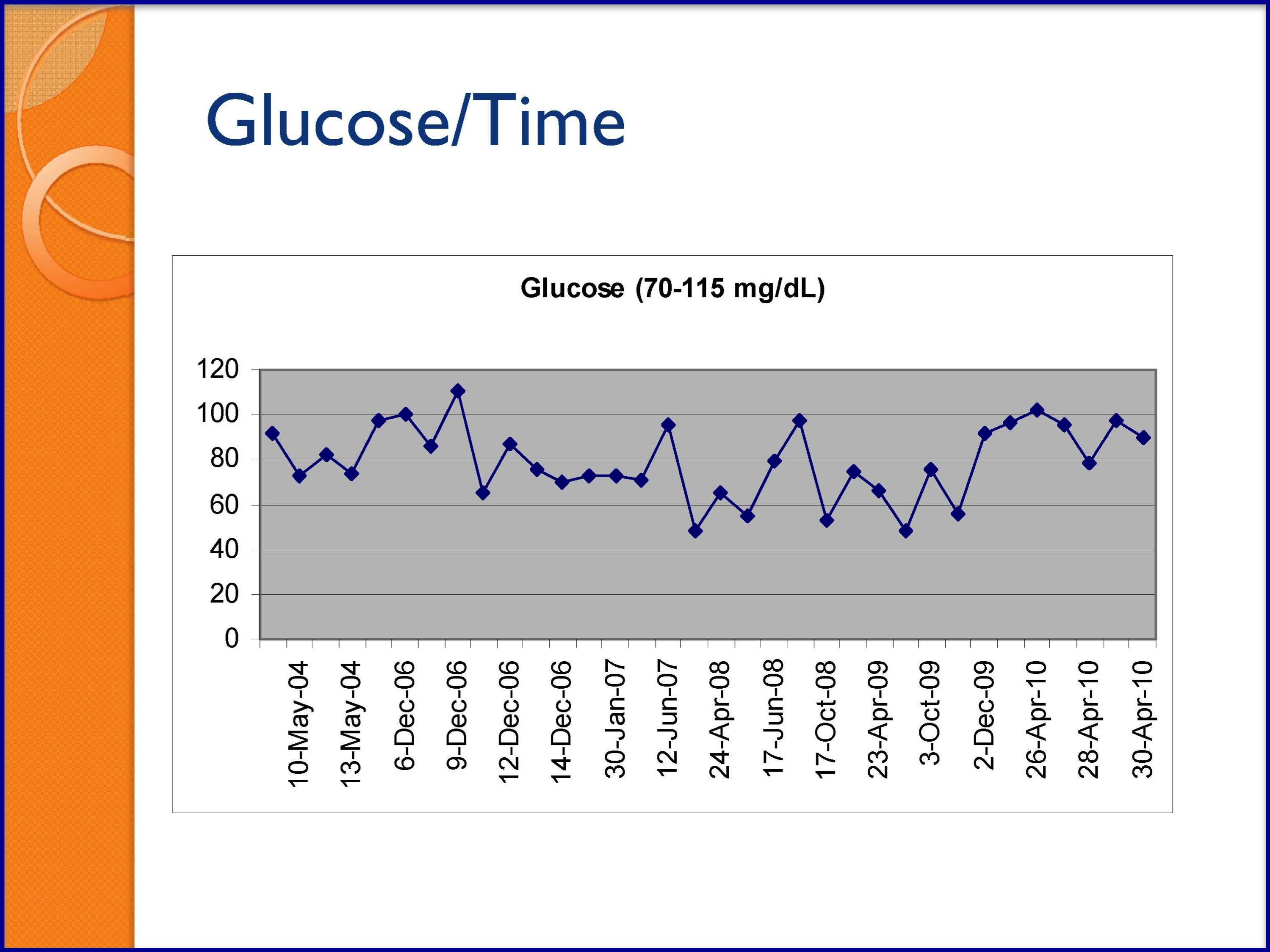
SLIDES 54-57
PART 2 (90 minutes)
SLIDE 59: Supplementary Resource—Webinar for Oral Health Screening in Primary Care Setting
- Integrating Oral Health Care in HIV Primary Care Settings: A Guide to Oral Health Care for PLWH is a web-based curriculum to train primary care providers on recognizing and managing oral health and disease for people living with HIV.
The objectives of the video are to enable viewers to:
- Describe the impact of oral health disease in PLWHA,
- Perform oral health screenings on HIV-infected patients, and
- Describe strategies for linking patients with HIV to dental care.
HANDOUT
Oral Health Assessment Tool
- Distribute copies of subjective data questionnaire to screen for oral health issues in HIV/AIDS patients at the end of class.
NURSES ORAL ASSESSMENT OF HIV/AIDS PATIENTS
Subjective Data Questions to Ask Patients: Dental History
- How often do you go to the dentist?
- What dental work have you had?
- Have you had any tooth extractions? Any post-op complications?
- Have you had previous orthodontic work?
- How many times a day do you brush or floss?
- Do you use a fluoride toothpaste or mouth rinse?
- Have you experienced any bleeding from your mouth or gums? How long?
- Do your gums bleed when you brush your teeth, floss, or eat?
- Do you wake up with blood on your pillow?
- Do you have dentures/dental appliances or braces?
- How do your dentures fit?
- Are there any areas of irritation in the gums under your dentures?
- How long do you wear your dentures at any one time?
- How do you care for your dentures?
- Have you had problems with speech or breathing?
- Do you have any loose teeth?
- Do you have difficulty chewing?
- Have you lost any teeth? How did it happen?
- Do you have or have you had lumps, redness, swelling, ulcers, blisters, sores, cracking, or pain on your:
– lips
– throat
– gums
– roof of mouth, back of mouth
– tongue
– sides of mouth?- Have you had any pain in your jaw? When does it occur? Describe it (e.g., severity, duration).
- Have you had any pain/swelling in your head, face, or neck? When? For how long?
- Do you have any swollen glands or lumps in your neck? Are they tender? Are they persistent or do they come and go? How long have you had them?
- Have you had any white patches in your mouth, or on your tongue?
- Do you have problems with food sticking in your throat or being difficult to swallow?
- Do you have or have you ever had a dry mouth, loss of taste, distortion of taste, or burning in your mouth?
- Have you had any trauma or burned your mouth? Describe it—appearance, severity, pain, location.
- Describe it (e.g., appearance, severity, pain, location).
- What do you take/do to relieve symptoms? Does it help?
- Is it constant or intermittent?
- Does it interfere with eating/drinking, swallowing, opening mouth? What foods do you avoid?
- Have you had any involuntary weight loss?
- Do you have toothaches? Do you have “cavities?” Where? How long? Describe them.
- Do you have any odor on your breath?
- Have you seen any dark spots on your gums, tongue, or other areas of your mouth?
- Where have you lived/traveled?
- Do you smoke or chew tobacco? How much? How long?
- Do you drink alcohol? How much? How long?
- Do you use cocaine/crack? How much? How long?
Source: Adapted from the AIDS Education and Training Center National Resource Center’s “HIV Oral Health Curriculum for Nursing Professionals.”