30 minutes
30 minutes
 PLAN module
PLAN module
Summary
This module provides an overview and will foster discussion about the HIV Interventions in Jails model of care. Participants will discuss the pros and cons of this model of care in targeting the marginalized and underserved PLWHA they wish to serve.
Materials Needed
- Computer and compatible LCD projector to play the PowerPoint presentation
- Notes created during previous modules
- Paper and easel(s)
- Colorful markers
- Tape for affixing paper to the wall as necessary
- Copies of the Module 7 handout to distribute
- Invited guest speaker(s), as needed.
Module 7 features teaching material, guided group discussion, and a group activity.
The Facilitator or other appointed person should write key thoughts voiced by participants throughout the presentation and subsequent discussions down on paper.
Before beginning the presentation, distribute the Module 7 handout, entitled HIV Interventions in Jails Logic Model.
The Facilitator should introduce the first slide, which serves as a refresher about the last session. If possible, affix the paper notes from the last module where they are visible to participants.
Slide #55: Training Refresher

 Before we begin, let’s review the pros and cons of the previous model we reviewed.
Before we begin, let’s review the pros and cons of the previous model we reviewed.
Slide #56: HIV Interventions in Jails
This model of care leverages the jail setting (and related correctional institutions such as parole offices) to identify and engage PLWHA into care.
The uniqueness of HIV care in jail settings involves its own model, which in part is a hybrid of several other models of care outlined in this curriculum.
Slide #57: What is the Difference Between a Jail and a Prison?
The terms “jail” and “prison” are often used interchangeably— but there are key distinctions.
- Prisons are State or Federal facilities that house people who have been convicted of a criminal or civil offense and sentenced to 1 year or more.
- Jails, however, are locally operated facilities whose inmates are typically sentenced to terms of 1 year or less, or are awaiting trial or sentencing following trial. The average jail stay is 10 to 20 days, according to the U.S. Department of Justice.
- Although jails have average daily populations that are half those of prisons, their populations experience greater turnover. The ratio of jail admissions to prison admissions is more than 16 to 1, and approximately 50 percent of people admitted to jails leave within 48 hours.
Slide #58: HIV Interventions in Jails Logic Model
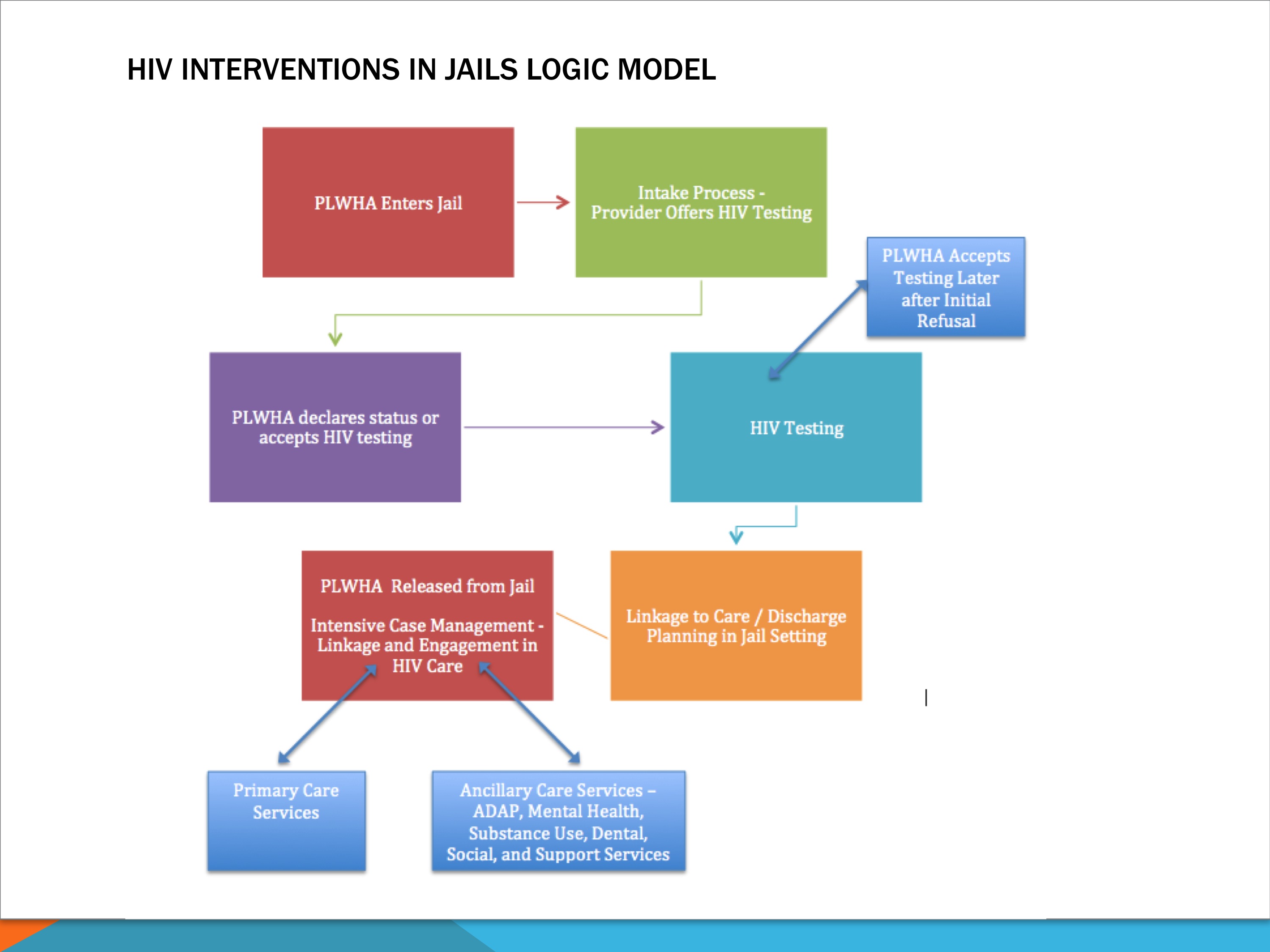
Here we have the HIV Interventions in Jails Logic Model.
We follow a patient from initial encounter to engagement in care.
Some things to keep in mind when adopting this model of care include:
- Socks make a great gift: Patient confidentiality in jails is limited. Greeting everyone with gifts of socks and/or underwear, as well as an offer of HIV testing, is a great way to make inmates feel less threatened by health-care workers.
Since everyone experiences the same encounter, it is impossible for staff and inmates to discern who decided to get tested for HIV and who did not.
PLWHA who do not wish to declare their status upfront to staff will opt for HIV testing as a backdoor to accessing care. - Ensure that inmates know they are not required to participate in testing. The atmosphere of corrections often makes everything, even health care, seem mandatory. Creating a set protocol will help reassure incarcerated persons of their rights.
- Time is of the essence: Jail stays often last only hours, so linkages to care must occur as soon as possible.
- Release = Another Chance for Engagement: Consider giving PLWHA a transitional care coordination package. This may include:
– A letter from the provider with all lab work results
– A packet of paperwork, such as AIDS Drug Assistance Program (ADAP) and/or Medicaid insurance applications
– A list of referrals
– Condoms and harm reduction/bleach kits
– Clothing
– Food
– Prescriptions
– Starter supply of medications. - Linkage upon release: Recently released PLWHA should be immediately connected with a case manager (sometimes an HSN) who helps get them engaged in care. Incentives, such as housing and other specialized services, may be used to help stabilize PLWHA released from jail settings into care.
- Don’t stop at HIV testing:Clinics with social workers on staff may want to consider working with courts to help vulnerable PLWHA be released to drug treatment facilities or monitored halfway houses.
Slide #59: Issues to Consider Before Working with Jails
Partnering with a jail can be challenging:
- Select jails closest to the clinic. Recently released PLWHA will be able to access services more easily.
- These are formal partnerships, generally based on an MOU. Jails often take the lead in these relationships, since the safety of inmates, staff, visitors, and the public is its responsibility.
- Jail administrators may view HIV testing as an administrative and staffing burden. To counter this issue, clinics should carefully outline what services they want to deliver.
– How many staff will be on site?
– What materials will be brought in?
– What services will you deliver?
– How long will patient consultations be?
– Consider having more than one staff person to ensure that all tasks are done in as little time, and with as minimal intrusion, as possible. - Alternative venues are just as powerful: Consider working with local probation and parole offices and other related agencies serving recently released inmates in the event that an agreement cannot be reached with the local jail system.
- There are potential hidden costs: There may be additional laboratory and staffing costs associated with this model of care. Costs often can be offset though partnerships with local and State health departments, and bulk purchasing contracts with vendors.
What are your experiences delivering HIV/AIDS care in a correctional setting?
Slide #60: Module 7 Activity: Q&A Quicktime
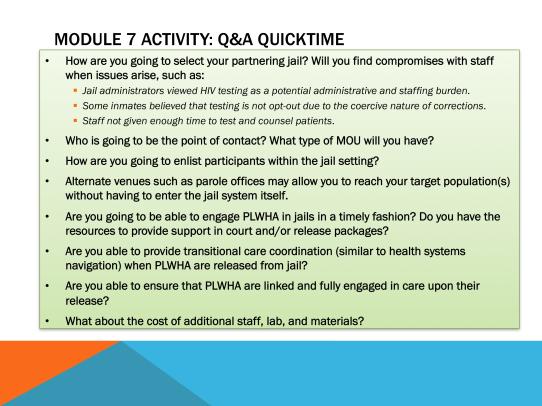
I am going to ask a question and then call on one of you to answer it. You have 2 seconds to respond —or to say “pass.”
Anyone who says “pass” has to ask a question of his/her own to someone else in the room. After that person answers, the “control” of the game returns to me for the next question.
I may ask questions that are not necessarily on this list, so
be ready!
Below are some game questions:
- How are you going to select your partnering jail?
- Will you find compromises with staff when issues inevitably arise, such as:
– Jail administrators view HIV testing as a potential administrative and staffing burden.
– Some inmates believe that testing is not opt-out due to the coercive nature of corrections.
– Staff are not given enough time to test and counsel patients.
If so, what other compromises do you anticipate?
- Who is going to be the point of contact?
- What type of MOU will you have?
- How are you going to enlist participants within the jail setting?
- Alternate venues such as parole offices may allow you to reach your target population(s) without having to enter the jail system itself.
- Are you going to be able to engage PLWHA in jails in a timely fashion? If so, how?
- Do you have the resources to provide support in court and/or release packages?
- Are you able to provide transitional care coordination (similar to health systems navigation) when PLWHA are released from jail?
- Will you be able to link and fully engage PLWHA in care before/after their release?
- What about the cost of additional staff, lab, and materials?
Lead the group evaluation discussion on whether this model of care will work for the clinic. Have participants refer to the Model of Care Evaluation Handout from Module 3.
Tape several pages of paper with the model of care’s title on each.
Slide #61: Group Module Evaluation

Read each question/statement and then write down everyone’s thoughts, questions, suggestions, etc. on paper.
- Can this model of care be readily integrated within the clinic’s current operations and help it reach targeted populations of PLWHA?
- Does the clinic already use this model of care, perhaps in a slightly different form?
- Can the clinic satisfy all requirements for this model of care?
- What funding streams, staffing, materials, and other resources are necessary to implement this model of care? Does the clinic have access to these? If not, how will it access them?
- How will buy-in be secured within the clinic?
- Will the implemented model of care be promoted to potential patients? If so, how? Online through social networks? Word of mouth?
- Does this model of care help the clinic identify and engage targeted PLWHA populations into care?
- Compare the pros and cons of this initiative with those of the modules.
If more than 10 people are present, the Facilitator can split participants into two or three groups to discuss the questions above and write their thoughts on paper. After a few minutes, the Facilitator should reconvene participants. Representatives from each group will explain their colleagues’ thoughts.
Save the paper from this and previous modules for reference in future sessions.